The world of healthcare is complex, and navigating the various processes involved in patient care can be overwhelming. One such process that can be particularly challenging is prior authorization, also known as pre-certification or pre-authorization. Prior authorization is a process by which healthcare providers obtain approval from a patient's insurance company before providing certain treatments, procedures, or prescription medications. This process can be time-consuming and may delay patient care if not managed efficiently. In this article, we will explore how Conifer Health Solutions can simplify the prior authorization process, making it easier for healthcare providers to focus on what matters most - patient care.
Understanding Prior Authorization
Prior authorization is a common practice in the healthcare industry, and its purpose is to ensure that patients receive necessary and cost-effective care. Insurance companies use prior authorization to review the medical necessity of a particular treatment or service before agreeing to cover it. While this process is intended to prevent unnecessary costs and ensure that patients receive evidence-based care, it can be a source of frustration for healthcare providers and patients alike.

The Challenges of Prior Authorization
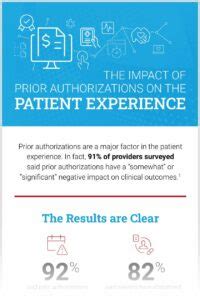
Prior authorization can be a complex and time-consuming process, involving multiple steps and stakeholders. Some of the common challenges associated with prior authorization include:
- Lengthy approval times: The prior authorization process can take several days or even weeks, delaying patient care and potentially impacting health outcomes.
- Administrative burdens: Healthcare providers often spend a significant amount of time and resources managing prior authorization requests, which can take away from patient care activities.
- Denials and appeals: Prior authorization requests can be denied, requiring healthcare providers to appeal the decision, which can add to the administrative burden and delay patient care.
- Lack of transparency: The prior authorization process can be opaque, making it difficult for healthcare providers to understand the status of their requests or the reasons for denials.
Simplifying Prior Authorization with Conifer Health Solutions
Conifer Health Solutions is a leading provider of healthcare solutions, including prior authorization services. Their approach to prior authorization is designed to simplify the process, reduce administrative burdens, and improve patient outcomes.

Streamlining Prior Authorization
Conifer Health Solutions uses advanced technology and expertise to streamline the prior authorization process. Their approach includes:
- Automated workflows: Conifer Health Solutions uses automated workflows to manage prior authorization requests, reducing the need for manual intervention and minimizing errors.
- Real-time tracking: Their system provides real-time tracking and updates, enabling healthcare providers to monitor the status of their requests and plan accordingly.
- Expert support: Conifer Health Solutions offers expert support and guidance throughout the prior authorization process, ensuring that healthcare providers receive the assistance they need to navigate complex insurance requirements.
Benefits of Conifer Health Solutions Prior Authorization
The benefits of using Conifer Health Solutions for prior authorization are numerous. Some of the advantages include:
- Reduced administrative burdens: Conifer Health Solutions manages the prior authorization process, freeing up healthcare providers to focus on patient care.
- Faster approval times: Their automated workflows and expert support enable faster approval times, reducing delays in patient care.
- Improved patient outcomes: By streamlining the prior authorization process, Conifer Health Solutions helps ensure that patients receive necessary treatments and services in a timely manner.

Case Studies and Success Stories
Conifer Health Solutions has helped numerous healthcare providers simplify their prior authorization processes. Here are a few case studies and success stories:
- A large hospital system reduced its prior authorization approval times by 50% after implementing Conifer Health Solutions' prior authorization services.
- A medical group practice increased its prior authorization approval rates by 25% with the help of Conifer Health Solutions' expert support and guidance.
Conclusion
Prior authorization can be a complex and time-consuming process, but it doesn't have to be. Conifer Health Solutions offers a simplified approach to prior authorization, leveraging advanced technology and expertise to reduce administrative burdens and improve patient outcomes. By streamlining the prior authorization process, healthcare providers can focus on what matters most - delivering high-quality patient care.

We invite you to share your thoughts and experiences with prior authorization in the comments below. How has your organization simplified the prior authorization process? What challenges have you faced, and how have you overcome them? Let's continue the conversation and explore ways to improve patient care through streamlined prior authorization processes.
What is prior authorization?
+Prior authorization, also known as pre-certification or pre-authorization, is a process by which healthcare providers obtain approval from a patient's insurance company before providing certain treatments, procedures, or prescription medications.
Why is prior authorization necessary?
+Prior authorization is necessary to ensure that patients receive necessary and cost-effective care. Insurance companies use prior authorization to review the medical necessity of a particular treatment or service before agreeing to cover it.
How can Conifer Health Solutions simplify the prior authorization process?
+Conifer Health Solutions uses advanced technology and expertise to streamline the prior authorization process, reducing administrative burdens and improving patient outcomes. Their approach includes automated workflows, real-time tracking, and expert support.