The CMS Form 2567 is a crucial document for healthcare providers who participate in the Centers for Medicare and Medicaid Services (CMS) programs. It is essential for providers to understand the purpose, components, and submission requirements of this form to ensure compliance and avoid potential penalties. In this article, we will delve into the details of the CMS Form 2567, its importance, and provide guidance on how to complete and submit it accurately.
What is the CMS Form 2567?

The CMS Form 2567, also known as the "Health Insurance Benefits Agreement," is a contract between healthcare providers and CMS. The form outlines the terms and conditions of participation in Medicare and Medicaid programs, including the provider's obligations, rights, and responsibilities. It is a mandatory document for all healthcare providers who want to participate in these programs and receive reimbursement for their services.
Why is the CMS Form 2567 important?
The CMS Form 2567 is essential for several reasons:
- It establishes a contractual relationship between the provider and CMS, outlining the terms and conditions of participation in Medicare and Medicaid programs.
- It ensures that providers understand their obligations and responsibilities, including compliance with program requirements, billing and payment rules, and patient rights.
- It helps providers to understand their rights, including the right to receive reimbursement for their services and to appeal adverse decisions.
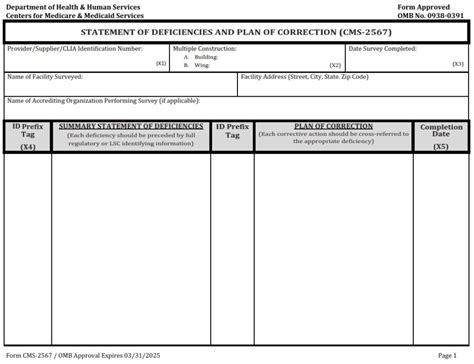
Components of the CMS Form 2567

The CMS Form 2567 consists of several sections, including:
- Section 1: Provider Information
- Section 2: Certification Statement
- Section 3: Terms and Conditions of Participation
- Section 4: Medicare and Medicaid Program Requirements
- Section 5: Billing and Payment Rules
- Section 6: Patient Rights and Responsibilities
- Section 7: Appeal Process
Section 1: Provider Information
This section requires providers to submit their contact information, including their name, address, and National Provider Identifier (NPI).
Section 2: Certification Statement
In this section, providers must certify that they have read and understood the terms and conditions of participation in Medicare and Medicaid programs.
Section 3: Terms and Conditions of Participation
This section outlines the provider's obligations and responsibilities, including compliance with program requirements, billing and payment rules, and patient rights.
Section 4: Medicare and Medicaid Program Requirements
This section details the specific requirements for participating in Medicare and Medicaid programs, including documentation, coding, and billing rules.
Section 5: Billing and Payment Rules
In this section, providers must agree to comply with CMS billing and payment rules, including the submission of accurate and timely claims.
Section 6: Patient Rights and Responsibilities
This section outlines the patient's rights and responsibilities, including the right to receive quality care, to be informed about their treatment, and to appeal adverse decisions.
Section 7: Appeal Process
In this section, providers must agree to comply with the appeal process for adverse decisions, including the submission of appeals and the provision of supporting documentation.
Submission Requirements for the CMS Form 2567

The CMS Form 2567 must be submitted electronically through the CMS website. Providers must ensure that they have a valid username and password to access the CMS portal.
Timing of Submission
The CMS Form 2567 must be submitted within 30 days of the provider's initial enrollment in Medicare and Medicaid programs. Providers who are re-enrolling in these programs must submit the form within 30 days of their re-enrollment date.
Verification of Submission
Providers must verify their submission of the CMS Form 2567 by printing and saving a copy of the confirmation page.
Penalties for Non-Compliance

Providers who fail to submit the CMS Form 2567 or who submit incomplete or inaccurate information may face penalties, including:
- Revocation of their Medicare and Medicaid enrollment
- Reimbursement withholding
- Civil monetary penalties
Conclusion
The CMS Form 2567 is a critical document for healthcare providers who participate in Medicare and Medicaid programs. Providers must understand the purpose, components, and submission requirements of this form to ensure compliance and avoid potential penalties. By completing and submitting the CMS Form 2567 accurately, providers can ensure that they are in compliance with CMS regulations and can provide quality care to their patients.
What is the purpose of the CMS Form 2567?
+The CMS Form 2567 is a contract between healthcare providers and CMS, outlining the terms and conditions of participation in Medicare and Medicaid programs.
What are the components of the CMS Form 2567?
+The CMS Form 2567 consists of several sections, including provider information, certification statement, terms and conditions of participation, Medicare and Medicaid program requirements, billing and payment rules, patient rights and responsibilities, and appeal process.
What are the penalties for non-compliance with the CMS Form 2567?
+Providers who fail to submit the CMS Form 2567 or who submit incomplete or inaccurate information may face penalties, including revocation of their Medicare and Medicaid enrollment, reimbursement withholding, and civil monetary penalties.