The world of healthcare is complex, and navigating the various forms and documents required for medical billing and insurance claims can be overwhelming. One crucial form in this process is the CMS-1490S form, which plays a significant role in ensuring accurate and efficient claims processing. In this article, we will delve into the intricacies of the CMS-1490S form, exploring its purpose, sections, and the importance of accurate completion.

The CMS-1490S form is a critical document used by healthcare providers to submit claims to Medicare and other insurance carriers. The form's primary purpose is to provide essential information about the patient, the services rendered, and the charges associated with those services. This information enables insurance carriers to process claims efficiently and accurately, ensuring timely reimbursement to healthcare providers.
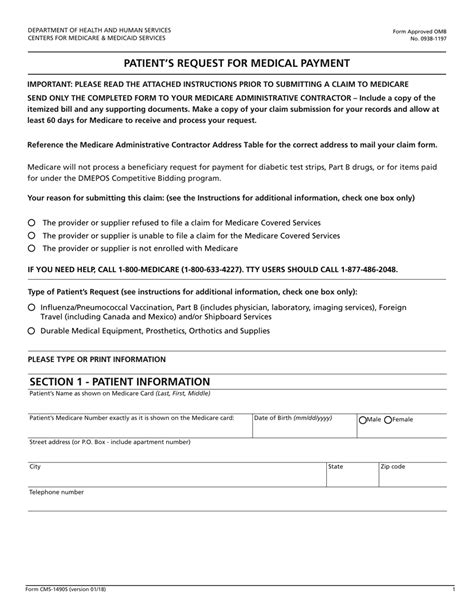
Breaking Down the CMS-1490S Form
The CMS-1490S form is divided into several sections, each requiring specific information. Understanding the purpose and requirements of each section is crucial for accurate completion.
Section 1: Patient Information
This section requires basic patient information, including name, date of birth, and insurance identification number. Accurate completion of this section is vital to ensure that the claim is processed correctly and that the patient receives the necessary benefits.
Section 2: Provider Information
In this section, healthcare providers must enter their name, address, and National Provider Identifier (NPI) number. This information is essential for insurance carriers to verify the provider's credentials and ensure that the claim is processed correctly.
Section 3: Services Rendered
This section requires a detailed description of the services rendered, including the dates of service, procedure codes, and charges associated with each service. Accurate completion of this section is critical to ensure that the claim is processed correctly and that the provider receives the correct reimbursement.

The Importance of Accurate Completion
Accurate completion of the CMS-1490S form is crucial to ensure efficient and accurate claims processing. Incomplete or inaccurate information can lead to delayed or denied claims, resulting in significant financial losses for healthcare providers. Moreover, accurate completion of the form is essential for compliance with regulatory requirements and to prevent potential audits or penalties.
Common Mistakes to Avoid
When completing the CMS-1490S form, healthcare providers must avoid common mistakes that can lead to delayed or denied claims. Some common mistakes include:
- Incomplete or inaccurate patient information
- Incorrect provider information
- Inaccurate or incomplete description of services rendered
- Incorrect charges or procedure codes

Tips for Efficient Claims Processing
To ensure efficient claims processing, healthcare providers can follow these tips:
- Verify patient information before submitting the claim
- Ensure accurate and complete provider information
- Use accurate and up-to-date procedure codes and charges
- Double-check the claim for completeness and accuracy before submission

Conclusion: Mastering the CMS-1490S Form
Mastering the CMS-1490S form is essential for healthcare providers to ensure accurate and efficient claims processing. By understanding the purpose and requirements of each section, avoiding common mistakes, and following tips for efficient claims processing, healthcare providers can minimize delays and denials, ensuring timely reimbursement and optimal patient care.

We hope this guide has provided valuable insights into the CMS-1490S form and its significance in the healthcare billing process. By following the tips and best practices outlined in this article, healthcare providers can optimize their claims processing and ensure timely reimbursement.
Share your thoughts and experiences with the CMS-1490S form in the comments below. Have you encountered any challenges or successes with claims processing? We'd love to hear from you!
What is the purpose of the CMS-1490S form?
+The CMS-1490S form is used by healthcare providers to submit claims to Medicare and other insurance carriers.
What information is required in Section 1 of the CMS-1490S form?
+Section 1 requires basic patient information, including name, date of birth, and insurance identification number.
What are some common mistakes to avoid when completing the CMS-1490S form?
+