The world of medical billing and insurance claims can be complex and overwhelming, especially for healthcare providers and patients alike. One of the most critical forms in this process is the CMS-1450 claim form, formerly known as the UB-04 claim form. This form is used to submit claims for reimbursement to Medicare, Medicaid, and other insurance providers. Accurate submission of the CMS-1450 claim form is essential to ensure timely and correct payment for healthcare services rendered.

In this article, we will delve into the intricacies of the CMS-1450 claim form, providing a comprehensive guide to accurate submission. We will cover the essential sections, required fields, and best practices to ensure a smooth claims process.
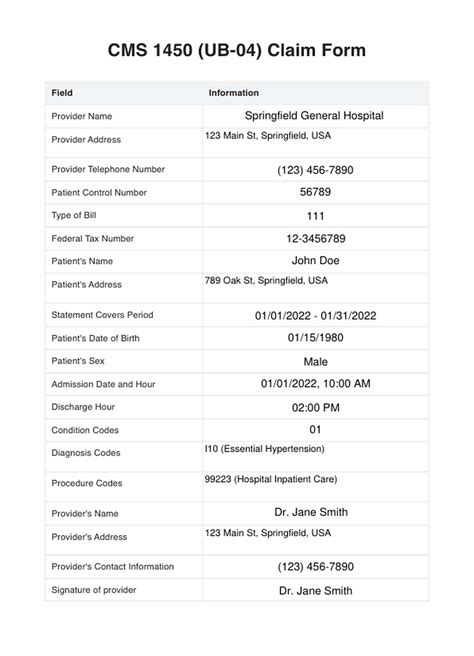
Understanding the CMS-1450 Claim Form
The CMS-1450 claim form is a standardized document used to report patient and billing information to insurance providers. The form is divided into several sections, each containing vital information necessary for claims processing.

The CMS-1450 claim form consists of the following sections:
- Header Section: This section contains information about the billing provider, patient, and claim.
- Patient Information Section: This section contains demographic information about the patient.
- Billing Provider Information Section: This section contains information about the billing provider.
- Service Information Section: This section contains information about the services rendered.
- Charges and Payments Section: This section contains information about the charges and payments.
Essential Sections and Required Fields
To ensure accurate submission, it is crucial to understand the essential sections and required fields on the CMS-1450 claim form.
- Patient Information Section:
- Patient Name (Field 1)
- Patient Address (Field 2)
- Patient Date of Birth (Field 3)
- Patient Sex (Field 4)
- Billing Provider Information Section:
- Billing Provider Name (Field 50)
- Billing Provider Address (Field 51)
- Billing Provider NPI (Field 56)
- Service Information Section:
- Service Dates (Field 45)
- Service Codes (Field 44)
- Service Charges (Field 47)
- Charges and Payments Section:
- Total Charges (Field 71)
- Total Payments (Field 72)

Best Practices for Accurate Submission
To ensure accurate submission of the CMS-1450 claim form, follow these best practices:
- Verify patient information, including name, address, and date of birth.
- Ensure accurate billing provider information, including name, address, and NPI.
- Use standardized service codes and descriptions.
- Double-check service dates and charges.
- Review total charges and payments for accuracy.

Common Errors and Rejections
Common errors and rejections on the CMS-1450 claim form include:
- Incomplete or inaccurate patient information
- Incorrect billing provider information
- Missing or invalid service codes
- Incorrect service dates or charges
- Mathematical errors in total charges and payments

Streamlining the Claims Process
To streamline the claims process, consider the following strategies:
- Implement an electronic claims submission system.
- Use claims scrubbing software to identify errors and inconsistencies.
- Establish a claims review process to ensure accuracy and completeness.
- Provide ongoing training and education for billing staff.

Conclusion and Next Steps
Accurate submission of the CMS-1450 claim form is crucial for timely and correct payment for healthcare services rendered. By understanding the essential sections and required fields, following best practices, and streamlining the claims process, healthcare providers can minimize errors and rejections.

We invite you to share your thoughts and experiences with the CMS-1450 claim form in the comments below. How have you overcome common errors and rejections? What strategies have you implemented to streamline the claims process?
What is the CMS-1450 claim form used for?
+The CMS-1450 claim form is used to submit claims for reimbursement to Medicare, Medicaid, and other insurance providers.
What are the essential sections on the CMS-1450 claim form?
+The essential sections on the CMS-1450 claim form include the Header Section, Patient Information Section, Billing Provider Information Section, Service Information Section, and Charges and Payments Section.
What are the most common errors and rejections on the CMS-1450 claim form?
+Common errors and rejections on the CMS-1450 claim form include incomplete or inaccurate patient information, incorrect billing provider information, missing or invalid service codes, incorrect service dates or charges, and mathematical errors in total charges and payments.