As a healthcare professional, you understand the importance of efficient documentation processes in providing quality patient care. One crucial aspect of this is the prior authorization (PA) process, which can be time-consuming and tedious. However, with the right tools and strategies, you can streamline your PA process and focus on what matters most – patient care.
In this article, we'll delve into the world of CCA prior auth forms, exploring the benefits, challenges, and best practices for simplifying your healthcare documentation process.
Understanding Prior Authorization (PA) and Its Importance

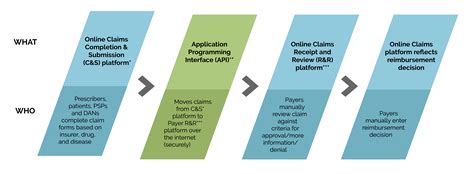
Prior authorization is a process used by healthcare payers to determine whether a specific treatment, service, or medication is medically necessary and covered under a patient's insurance plan. The PA process involves submitting a request to the payer, who reviews the request and makes a determination.
While PA is intended to ensure that patients receive necessary and effective care, it can be a complex and time-consuming process, leading to delays in treatment and frustration for both patients and providers.
The Challenges of Prior Authorization

Despite its importance, the PA process is often plagued by inefficiencies, including:
- Manual data entry and paperwork
- Incomplete or inaccurate submissions
- Delays in processing and approval
- Lack of transparency and communication
These challenges can lead to increased administrative burdens, decreased productivity, and compromised patient care.
Introducing CCA Prior Auth Forms: A Solution to Streamline Your PA Process

CCA prior auth forms are designed to simplify and streamline the PA process, reducing administrative burdens and improving patient outcomes. These forms are specifically designed to:
- Automate data entry and submission
- Ensure accuracy and completeness
- Expedite processing and approval
- Enhance transparency and communication
By leveraging CCA prior auth forms, healthcare providers can:
- Reduce administrative time and costs
- Improve patient satisfaction and outcomes
- Enhance collaboration and communication with payers
Benefits of Using CCA Prior Auth Forms

The benefits of using CCA prior auth forms are numerous, including:
- Increased efficiency and productivity
- Improved accuracy and reduced errors
- Enhanced patient satisfaction and outcomes
- Reduced administrative burdens and costs
- Improved collaboration and communication with payers
Best Practices for Implementing CCA Prior Auth Forms

To ensure a successful implementation of CCA prior auth forms, consider the following best practices:
- Automate data entry and submission
- Ensure accuracy and completeness
- Establish clear communication channels with payers
- Monitor and track PA requests and outcomes
- Continuously evaluate and improve the PA process
Overcoming Common Challenges and Obstacles

While CCA prior auth forms can simplify the PA process, there may still be challenges and obstacles to overcome, including:
- Resistance to change
- Technical issues and integration challenges
- Limited resources and support
- Payer-specific requirements and regulations
To overcome these challenges, consider:
- Providing education and training on CCA prior auth forms
- Establishing clear communication channels with payers
- Ensuring technical support and resources are available
- Continuously monitoring and evaluating the PA process
Conclusion: Simplifying Your Healthcare Documentation Process with CCA Prior Auth Forms

By implementing CCA prior auth forms, healthcare providers can simplify and streamline the PA process, reducing administrative burdens and improving patient outcomes. By understanding the benefits, challenges, and best practices for using CCA prior auth forms, providers can take the first step towards a more efficient and effective healthcare documentation process.
We invite you to share your thoughts and experiences with CCA prior auth forms in the comments below. How have you simplified your PA process? What challenges have you faced, and how have you overcome them?
What are CCA prior auth forms?
+CCA prior auth forms are specifically designed to simplify and streamline the prior authorization process, reducing administrative burdens and improving patient outcomes.
How can CCA prior auth forms benefit my practice?
+CCA prior auth forms can benefit your practice by increasing efficiency and productivity, improving accuracy and reducing errors, and enhancing patient satisfaction and outcomes.
How do I implement CCA prior auth forms in my practice?
+To implement CCA prior auth forms, consider automating data entry and submission, ensuring accuracy and completeness, establishing clear communication channels with payers, and continuously evaluating and improving the PA process.