Receiving a denial of coverage from CareSource can be a stressful and overwhelming experience, especially when you or a loved one is in need of medical treatment. However, there is hope for reversing the decision through the appeals process. Understanding the CareSource appeal form and the step-by-step process can help you navigate this challenging situation and increase your chances of a successful outcome.

The CareSource appeal form is a formal document that allows you to contest the denial of coverage and provide additional information to support your claim. In this article, we will guide you through the process of completing the appeal form, gathering required documents, and submitting your appeal.
Understanding the CareSource Appeal Process
Before we dive into the step-by-step guide, it's essential to understand the CareSource appeal process. The process typically involves the following stages:
-
Initial Review
CareSource reviews your initial claim and makes a determination regarding coverage.
-
Appeal Filing
You file an appeal, providing additional information to support your claim.
-
Reconsideration
CareSource re-evaluates your claim, taking into account the new information provided.
-
Final Determination
CareSource makes a final decision regarding coverage.
Step 1: Gather Required Documents
To complete the CareSource appeal form, you will need to gather the following documents:
- A copy of the denial letter or notification
- Your CareSource member ID card
- Medical records and documentation supporting your claim
- A written statement explaining why you disagree with the denial
- Any additional information or evidence that supports your appeal

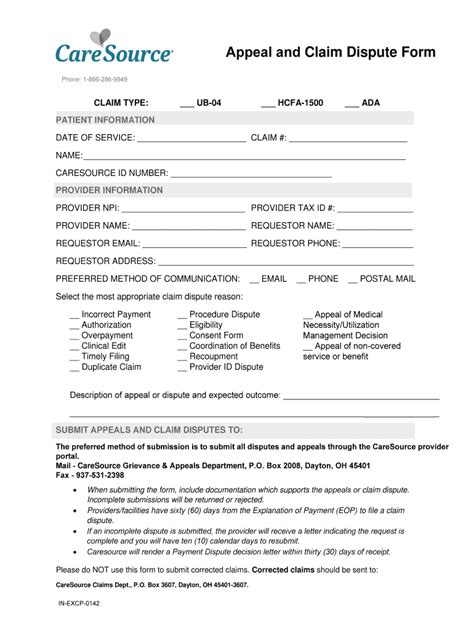
Step 2: Complete the CareSource Appeal Form
The CareSource appeal form can be obtained by:
- Downloading it from the CareSource website
- Contacting CareSource customer service
- Requesting a form through the mail
Once you have the form, follow these steps:
- Section 1: Provide your personal and contact information
- Section 2: Enter your CareSource member ID number and the date of the denial letter
- Section 3: Explain why you disagree with the denial and provide supporting evidence
- Section 4: Attach all required documents and supporting evidence
Tips for Completing the Appeal Form
- Be clear and concise in your explanation
- Provide detailed information about your medical condition and treatment
- Include all relevant medical records and documentation
- Proofread your form for accuracy and completeness

Step 3: Submit Your Appeal
Once you have completed the appeal form and gathered all required documents, submit your appeal to CareSource. You can submit your appeal by:
- Mail: CareSource, Attn: Appeals Department, [insert address]
- Fax: [insert fax number]
- Email: [insert email address]
Tracking Your Appeal
After submitting your appeal, you can track the status of your appeal by:
- Contacting CareSource customer service
- Checking your online account
- Requesting a status update through the mail
Additional Tips and Reminders
- Keep a copy of your appeal form and supporting documents for your records
- Follow up with CareSource to ensure they have received your appeal
- Be patient and persistent throughout the appeals process
- Consider seeking assistance from a patient advocate or healthcare professional

By following these steps and tips, you can effectively navigate the CareSource appeal process and increase your chances of a successful outcome. Remember to stay patient, persistent, and informed throughout the process.
We encourage you to share your experiences and ask questions in the comments below. Your feedback will help us improve our content and provide better support for our readers.
What is the CareSource appeal process?
+The CareSource appeal process is a formal procedure that allows you to contest a denial of coverage and provide additional information to support your claim.
How do I obtain a CareSource appeal form?
+You can obtain a CareSource appeal form by downloading it from the CareSource website, contacting CareSource customer service, or requesting a form through the mail.
What documents do I need to submit with my appeal?
+You will need to submit a copy of the denial letter or notification, your CareSource member ID card, medical records and documentation supporting your claim, a written statement explaining why you disagree with the denial, and any additional information or evidence that supports your appeal.