The healthcare system can be complex and overwhelming, especially when it comes to managing medical treatments and accessing necessary care. One crucial aspect of this system is prior authorization, a process that ensures patients receive the most effective and cost-efficient care possible. For Carelon patients, navigating this process can be streamlined with the use of a prior authorization form. In this comprehensive guide, we will delve into the world of Carelon prior authorization, providing an easy-to-understand overview, a step-by-step guide, and information on how to download the necessary form.
Understanding Carelon Prior Authorization

Prior authorization is a process used by healthcare providers and insurance companies to determine whether a specific treatment or medication is medically necessary and covered under a patient's insurance plan. This process helps to prevent unnecessary treatments, reduce healthcare costs, and ensure that patients receive the most effective care possible. Carelon, a leading healthcare management company, utilizes prior authorization to facilitate the delivery of high-quality, patient-centered care.
Benefits of Prior Authorization
The prior authorization process offers several benefits to patients, healthcare providers, and insurance companies. Some of the key advantages include:
- Ensures medically necessary care: Prior authorization helps to guarantee that patients receive treatments and medications that are essential to their health and well-being.
- Reduces healthcare costs: By preventing unnecessary treatments and medications, prior authorization can help to lower healthcare costs and reduce financial burdens on patients and insurance companies.
- Improves patient outcomes: By ensuring that patients receive the most effective care possible, prior authorization can lead to better health outcomes and improved quality of life.
The Carelon Prior Authorization Process

The Carelon prior authorization process is designed to be efficient and patient-centered. Here's a step-by-step guide to help you understand the process:
- Initial Request: The healthcare provider submits a prior authorization request to Carelon, providing detailed information about the patient's condition, treatment plan, and medical necessity.
- Review and Verification: Carelon's team of medical professionals reviews the request, verifying the patient's eligibility and the medical necessity of the treatment or medication.
- Approval or Denial: Carelon makes a determination regarding the prior authorization request, either approving or denying the request.
- Notification: Carelon notifies the healthcare provider and patient of the prior authorization decision, providing clear explanations and instructions for next steps.
Required Information for Prior Authorization
To ensure a smooth prior authorization process, it's essential to provide the required information. Some of the key details include:
- Patient demographics and insurance information
- Medical history and diagnosis
- Treatment plan and medication details
- Clinical notes and test results
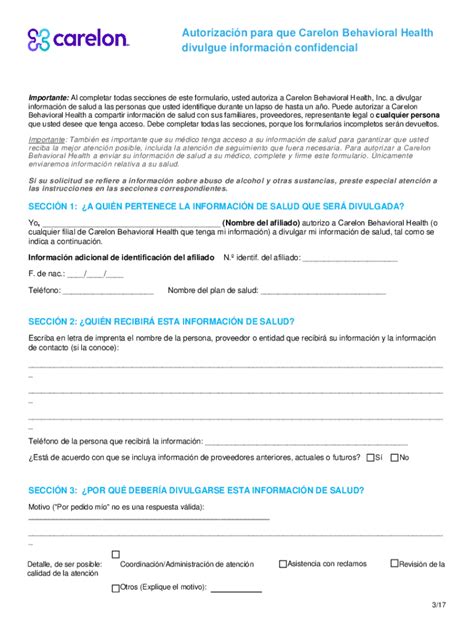
Downloading the Carelon Prior Authorization Form

The Carelon prior authorization form can be downloaded from the Carelon website or obtained from your healthcare provider. The form typically includes the following sections:
- Patient information
- Medical history and diagnosis
- Treatment plan and medication details
- Healthcare provider information
- Authorization and consent
Tips for Completing the Prior Authorization Form
When completing the prior authorization form, keep the following tips in mind:
- Ensure all sections are completed accurately and thoroughly
- Provide clear and concise information about the patient's condition and treatment plan
- Attach all required documentation, including clinical notes and test results
- Review the form carefully before submitting it to Carelon
Frequently Asked Questions
What is prior authorization?
+Prior authorization is a process used by healthcare providers and insurance companies to determine whether a specific treatment or medication is medically necessary and covered under a patient's insurance plan.
How do I obtain a prior authorization form?
+The Carelon prior authorization form can be downloaded from the Carelon website or obtained from your healthcare provider.
What information do I need to provide for prior authorization?
+Required information includes patient demographics and insurance information, medical history and diagnosis, treatment plan and medication details, and clinical notes and test results.
By understanding the Carelon prior authorization process and using the provided form, patients and healthcare providers can ensure a smooth and efficient experience. Remember to provide accurate and complete information, and don't hesitate to reach out to Carelon with any questions or concerns.
Share your experiences or ask questions about the Carelon prior authorization process in the comments below!