Prior authorization, also known as pre-authorization or pre-certification, is a process that healthcare providers must navigate before administering certain treatments, tests, or medications to patients. The process can be lengthy, bureaucratic, and frustrating for all parties involved, from patients to healthcare providers to insurance companies. Care coordinators by Quantum Health are changing the landscape of prior authorization by simplifying the process. In this article, we'll delve into the five ways care coordinators by Quantum Health make prior authorization more efficient and less complicated.
Understanding Prior Authorization: A Brief Overview
Prior authorization is a critical component of the healthcare system, aimed at ensuring that patients receive necessary treatments while minimizing unnecessary costs. Healthcare providers must obtain approval from insurance companies before performing certain procedures or prescribing specific medications. This process helps prevent unnecessary treatments, reduces healthcare costs, and ensures that patients receive the most effective and efficient care.

Challenges Associated with Prior Authorization
While prior authorization is essential, the process can be challenging and time-consuming. Healthcare providers often struggle with:
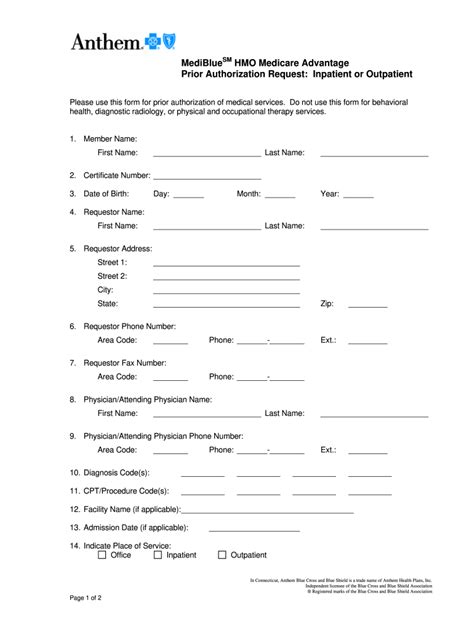
- Multiple phone calls and faxes to insurance companies
- Complex paperwork and documentation requirements
- Long wait times for approval or denial
- Difficulty understanding insurance company policies and requirements
- Managing denials and appeals
These challenges can lead to delayed treatments, increased costs, and frustrated patients.
Streamlining Prior Authorization: The Role of Care Coordinators
Care coordinators by Quantum Health are trained professionals who specialize in navigating the prior authorization process. They work closely with healthcare providers, insurance companies, and patients to simplify the process and ensure timely approval. Here are five ways care coordinators by Quantum Health simplify prior authorization:
1. Centralized Communication and Documentation
Care coordinators by Quantum Health act as a single point of contact for all stakeholders involved in the prior authorization process. They manage communication, documentation, and paperwork, reducing the administrative burden on healthcare providers. By centralizing communication, care coordinators ensure that all parties are informed and up-to-date, minimizing delays and miscommunications.

2. Expert Knowledge of Insurance Company Policies
Care coordinators by Quantum Health have in-depth knowledge of insurance company policies, procedures, and requirements. They understand the intricacies of prior authorization and can efficiently navigate the process. By leveraging their expertise, care coordinators can reduce the risk of denials and appeals, ensuring that patients receive timely approval for necessary treatments.
Reducing Denials and Appeals
Care coordinators by Quantum Health can help reduce denials and appeals by:
- Ensuring accurate and complete documentation
- Understanding insurance company policies and requirements
- Proactively addressing potential issues or concerns
By minimizing denials and appeals, care coordinators can reduce the administrative burden on healthcare providers and insurance companies, ultimately benefiting patients.
3. Real-Time Status Updates and Tracking
Care coordinators by Quantum Health provide real-time status updates and tracking, ensuring that all stakeholders are informed about the progress of prior authorization requests. This transparency helps reduce anxiety and uncertainty, allowing patients to focus on their treatment plans.

4. Personalized Support and Guidance
Care coordinators by Quantum Health offer personalized support and guidance to patients, healthcare providers, and insurance companies. They address concerns, answer questions, and provide education on the prior authorization process. By offering tailored support, care coordinators can alleviate stress and frustration, ensuring a smoother experience for all parties involved.
Supporting Patients and Families
Care coordinators by Quantum Health can also provide emotional support and guidance to patients and families, helping them navigate the complexities of prior authorization. By offering a listening ear and expert advice, care coordinators can reduce anxiety and uncertainty, ultimately improving patient satisfaction.
5. Analyzing and Optimizing Prior Authorization Workflows
Care coordinators by Quantum Health analyze and optimize prior authorization workflows, identifying areas for improvement and implementing process enhancements. By streamlining workflows, care coordinators can reduce administrative burdens, minimize delays, and improve overall efficiency.

Conclusion: Simplifying Prior Authorization with Care Coordinators
Prior authorization can be a complex and time-consuming process, but care coordinators by Quantum Health are changing the landscape. By centralizing communication, leveraging expert knowledge, reducing denials and appeals, providing real-time status updates, offering personalized support, and analyzing workflows, care coordinators can simplify prior authorization and improve the overall healthcare experience.

Take the First Step: Partner with Care Coordinators
If you're a healthcare provider, insurance company, or patient looking to simplify prior authorization, consider partnering with care coordinators by Quantum Health. Their expertise, guidance, and support can help reduce administrative burdens, minimize delays, and improve overall efficiency.

What is prior authorization, and why is it necessary?
+Prior authorization is a process that healthcare providers must navigate before administering certain treatments, tests, or medications to patients. It ensures that patients receive necessary treatments while minimizing unnecessary costs.
What are the benefits of working with care coordinators for prior authorization?
+Care coordinators can simplify the prior authorization process, reduce administrative burdens, minimize delays, and improve overall efficiency. They provide expert knowledge, guidance, and support to patients, healthcare providers, and insurance companies.
How can care coordinators reduce denials and appeals?
+Care coordinators can reduce denials and appeals by ensuring accurate and complete documentation, understanding insurance company policies and requirements, and proactively addressing potential issues or concerns.