The Buckeye Prior Authorization (PA) process can be a daunting task for healthcare providers, especially when it comes to filling out the necessary forms. However, with a clear understanding of the requirements and a step-by-step approach, navigating the Buckeye Prior Auth Form can be a straightforward process.
Prior authorization is a crucial step in ensuring that patients receive the necessary medical treatment while also managing healthcare costs. The Buckeye Prior Auth Form is a critical component of this process, and its accurate completion is essential for facilitating timely and effective patient care.
In this article, we will delve into the world of Buckeye Prior Authorization, providing a comprehensive guide to help healthcare providers navigate the process with ease. We will explore the importance of prior authorization, the role of the Buckeye Prior Auth Form, and provide a step-by-step walkthrough of the form's completion.
What is Prior Authorization?
Prior authorization is a process used by health insurance companies to determine whether a specific medical treatment or service is medically necessary and covered under a patient's insurance plan. The process involves reviewing the patient's medical history, diagnosis, and treatment plan to ensure that the requested service is necessary and aligns with the insurance company's policies.
Prior authorization is an essential step in managing healthcare costs and ensuring that patients receive the most effective and efficient treatment. By reviewing treatment plans and medical necessity, insurance companies can help reduce unnecessary medical expenses and promote high-quality patient care.
The Role of the Buckeye Prior Auth Form
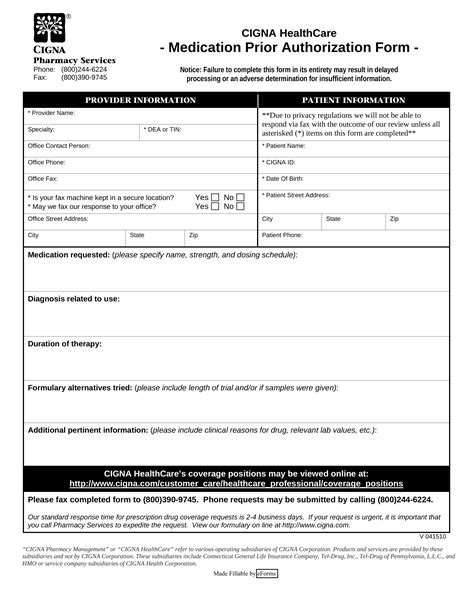
The Buckeye Prior Auth Form is a critical component of the prior authorization process. The form is used by healthcare providers to request prior authorization for specific medical treatments or services. The form requires providers to submit detailed information about the patient's medical condition, treatment plan, and supporting documentation.
The Buckeye Prior Auth Form is used to:
- Request prior authorization for medical treatments or services
- Provide detailed information about the patient's medical condition and treatment plan
- Submit supporting documentation, such as medical records and test results
- Facilitate communication between healthcare providers and insurance companies
Step-by-Step Guide to Completing the Buckeye Prior Auth Form
Completing the Buckeye Prior Auth Form requires attention to detail and a thorough understanding of the patient's medical condition and treatment plan. Here is a step-by-step guide to help healthcare providers navigate the form:
Section 1: Patient Information
- Patient Name: Enter the patient's full name
- Date of Birth: Enter the patient's date of birth
- Insurance ID Number: Enter the patient's insurance ID number

Section 2: Medical Information
- Diagnosis: Enter the patient's diagnosis or medical condition
- ICD-10 Code: Enter the relevant ICD-10 code
- Medical Condition Description: Provide a brief description of the patient's medical condition

Section 3: Treatment Information
- Treatment Requested: Enter the specific treatment or service being requested
- NDC Code: Enter the relevant NDC code (if applicable)
- Dose and Frequency: Enter the dose and frequency of the treatment

Section 4: Supporting Documentation
- Attach supporting documentation, such as medical records and test results

Section 5: Certification and Signature
- Certify that the information provided is accurate and complete
- Sign and date the form

Tips and Best Practices
- Ensure accurate and complete information to avoid delays or denials
- Attach all supporting documentation to facilitate the review process
- Use clear and concise language when describing the patient's medical condition and treatment plan
- Verify the patient's insurance coverage and policy details before submitting the form
Conclusion
Completing the Buckeye Prior Auth Form requires attention to detail and a thorough understanding of the patient's medical condition and treatment plan. By following this step-by-step guide, healthcare providers can ensure accurate and complete submissions, facilitating timely and effective patient care.
We encourage healthcare providers to share their experiences and tips for completing the Buckeye Prior Auth Form in the comments below. Your feedback and insights will help us improve this guide and provide better support for healthcare providers.
What is prior authorization?
+Prior authorization is a process used by health insurance companies to determine whether a specific medical treatment or service is medically necessary and covered under a patient's insurance plan.
What is the purpose of the Buckeye Prior Auth Form?
+The Buckeye Prior Auth Form is used by healthcare providers to request prior authorization for specific medical treatments or services.
What information is required to complete the Buckeye Prior Auth Form?
+The form requires patient information, medical information, treatment information, supporting documentation, and certification and signature.