Navigating the complexities of Medicaid prior authorization can be a daunting task, especially for healthcare providers and patients relying on Blue Cross Community Illinois Medicaid. Prior authorization, also known as pre-authorization, is a process where a healthcare provider must obtain approval from the patient's insurance company before providing certain medical treatments, services, or prescription medications. This process is designed to ensure that patients receive necessary and cost-effective care, but it can often lead to delays and frustration. In this article, we will delve into the specifics of Blue Cross Community Illinois Medicaid prior auth, providing tips and insights to help streamline the process for both healthcare providers and patients.
Understanding Blue Cross Community Illinois Medicaid Prior Auth
Blue Cross Community Illinois Medicaid is a Medicaid managed care program offered by Blue Cross and Blue Shield of Illinois (BCBSIL). The program provides healthcare coverage to low-income individuals and families, including children, pregnant women, and people with disabilities. As with any Medicaid program, prior authorization is a critical component of ensuring that patients receive medically necessary care while controlling costs.
Tip 1: Know the Prior Authorization Requirements
To avoid delays and denials, it's essential to understand the prior authorization requirements for Blue Cross Community Illinois Medicaid. Healthcare providers should familiarize themselves with the program's prior authorization policy, which outlines the specific services, treatments, and medications that require prior authorization. This information can be found on the BCBSIL website or by contacting the program's customer service department.

Some common services that require prior authorization under Blue Cross Community Illinois Medicaid include:
- Inpatient hospital admissions
- Outpatient surgeries
- Certain prescription medications
- Durable medical equipment (DME)
- Home health services
Tip 2: Submit Complete and Accurate Information
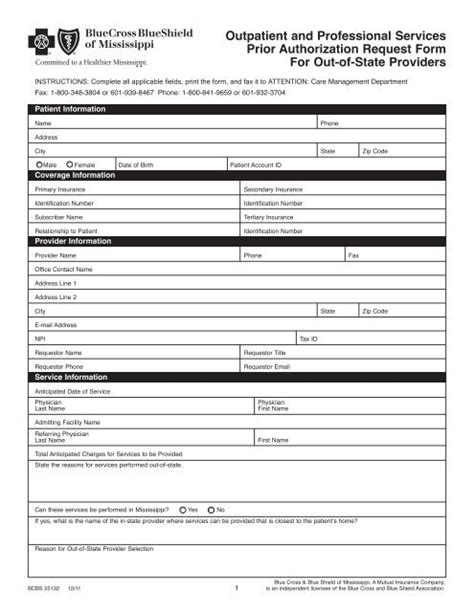
When submitting a prior authorization request, it's crucial to provide complete and accurate information. This includes:
- Patient demographics and insurance information
- Diagnosis and treatment plan
- Medical records and test results
- Provider contact information
Inaccurate or incomplete information can lead to delays or denials, so it's essential to double-check the submission before sending it to BCBSIL.
Blue Cross Community Illinois Medicaid Prior Auth Process
The prior authorization process for Blue Cross Community Illinois Medicaid involves several steps:
- Submission: The healthcare provider submits a prior authorization request to BCBSIL, either online or by phone.
- Review: BCBSIL reviews the request to determine if the requested service or treatment meets the program's medical necessity criteria.
- Determination: BCBSIL makes a determination and notifies the healthcare provider and patient of the outcome.

Tip 3: Use the Online Portal for Faster Processing
BCBSIL offers an online portal for healthcare providers to submit prior authorization requests. This portal, known as the Blue Cross Community Illinois Medicaid Prior Authorization Portal, allows providers to submit requests electronically, reducing the risk of errors and delays.
Tip 4: Follow Up on Pending Requests
If a prior authorization request is pending, it's essential to follow up with BCBSIL to ensure that the request is being processed in a timely manner. Healthcare providers can use the online portal or contact BCBSIL's customer service department to check the status of a pending request.
Common Prior Authorization Denials and How to Avoid Them
Prior authorization denials can occur for various reasons, including:
- Lack of medical necessity: The requested service or treatment does not meet the program's medical necessity criteria.
- Incomplete or inaccurate information: The prior authorization request lacks essential information or contains errors.
To avoid denials, healthcare providers should ensure that the prior authorization request is complete and accurate and that the requested service or treatment meets the program's medical necessity criteria.

Tip 5: Appeal a Denied Prior Authorization Request
If a prior authorization request is denied, healthcare providers can appeal the decision. The appeal process involves submitting additional information or clarification to support the original request. It's essential to understand the appeal process and deadlines to ensure that the patient receives the necessary care.
Conclusion
Navigating the Blue Cross Community Illinois Medicaid prior authorization process can be complex, but by following these tips, healthcare providers and patients can streamline the process and ensure that necessary care is received in a timely manner. Remember to understand the prior authorization requirements, submit complete and accurate information, use the online portal, follow up on pending requests, and appeal denied requests.

We encourage you to share your experiences and tips for navigating the Blue Cross Community Illinois Medicaid prior authorization process in the comments below. By working together, we can ensure that patients receive the care they need while minimizing delays and frustration.
FAQ Section
What is prior authorization, and why is it required?
+Prior authorization is a process where a healthcare provider must obtain approval from the patient's insurance company before providing certain medical treatments, services, or prescription medications. It's designed to ensure that patients receive necessary and cost-effective care.
What services require prior authorization under Blue Cross Community Illinois Medicaid?
+Common services that require prior authorization include inpatient hospital admissions, outpatient surgeries, certain prescription medications, durable medical equipment (DME), and home health services.
How can I appeal a denied prior authorization request?
+If a prior authorization request is denied, healthcare providers can appeal the decision by submitting additional information or clarification to support the original request. It's essential to understand the appeal process and deadlines to ensure that the patient receives the necessary care.