As a healthcare provider or patient, navigating the complexities of prior authorization forms can be overwhelming, especially when dealing with Blue Cross Blue Shield of Texas (BCBS TX). The prior authorization process is designed to ensure that patients receive necessary and cost-effective care, but it can be a time-consuming and frustrating experience. In this article, we will break down the BCBS TX prior authorization form into 5 easy steps, making it more manageable for you.
Understanding the Importance of Prior Authorization

Prior authorization is a crucial step in the healthcare process that ensures patients receive necessary and cost-effective care. It involves submitting a request to BCBS TX for approval before providing certain medical services or treatments. This process helps to reduce unnecessary medical costs, ensures that patients receive evidence-based treatments, and prevents unnecessary hospitalizations.
Step 1: Determine If Prior Authorization Is Required

Before starting the prior authorization process, it's essential to determine if it's required for the specific medical service or treatment. You can check the BCBS TX website or contact their customer service to confirm if prior authorization is needed. Some medical services, such as emergency care, do not require prior authorization.
Services That Typically Require Prior Authorization
- Specialty medications
- Surgical procedures
- Hospitalizations
- Imaging services (e.g., MRI, CT scans)
- Durable medical equipment
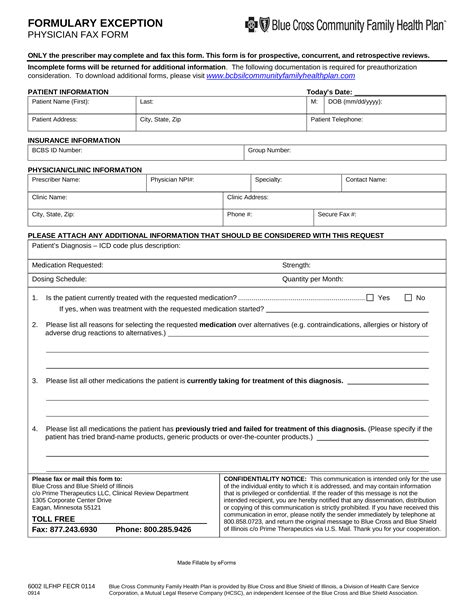
Step 2: Gather Required Information and Documents

To complete the prior authorization form, you'll need to gather specific information and documents, including:
- Patient's demographics and medical history
- Medical service or treatment requested
- Diagnosis and treatment plan
- Supporting medical documentation (e.g., test results, medical records)
- Prescriptions or medication lists
Tips for Gathering Required Information
- Ensure that all patient information is accurate and up-to-date
- Collect all relevant medical documentation and test results
- Verify the patient's eligibility and benefits with BCBS TX
Step 3: Complete the Prior Authorization Form

Once you have gathered all the required information and documents, it's time to complete the prior authorization form. You can download the form from the BCBS TX website or request one from their customer service. Make sure to fill out the form accurately and thoroughly, as incomplete or inaccurate information may lead to delays or denials.
Key Sections of the Prior Authorization Form
- Patient demographics and medical history
- Medical service or treatment requested
- Diagnosis and treatment plan
- Supporting medical documentation
- Signature and date
Step 4: Submit the Prior Authorization Request

After completing the prior authorization form, submit it to BCBS TX via fax, email, or online portal. Ensure that you follow the correct submission guidelines and deadlines to avoid delays.
Submission Methods
- Fax: 1-800-626-0749
- Email:
- Online Portal: Availity or Blue Cross Blue Shield of Texas Provider Portal
Step 5: Follow Up on the Prior Authorization Request

After submitting the prior authorization request, follow up with BCBS TX to ensure that it has been received and processed. You can check the status of the request online or by contacting their customer service.
Tips for Following Up
- Verify that the request has been received and is being processed
- Check the status of the request online or by phone
- Respond promptly to any additional information requests
By following these 5 easy steps, you can simplify the BCBS TX prior authorization form process and ensure that your patients receive the necessary medical care. Remember to stay organized, gather all required information and documents, and follow up on the prior authorization request to avoid delays or denials.
What is prior authorization, and why is it required?
+Prior authorization is a process that ensures patients receive necessary and cost-effective care. It's required for certain medical services or treatments to ensure that they are medically necessary and meet specific criteria.
How long does the prior authorization process take?
+The prior authorization process typically takes 2-5 business days, but it may vary depending on the complexity of the request and the availability of necessary information.
What happens if the prior authorization request is denied?
+If the prior authorization request is denied, you can appeal the decision by submitting additional information or documentation to support the request.