Healthcare providers and patients alike often find themselves entangled in the complex process of prior authorization (prior auth) when dealing with insurance companies. One of the largest and most prominent health insurance providers in the United States is Blue Cross Blue Shield (BCBS). Navigating the prior auth process can be daunting, especially when dealing with a large organization like BCBS. However, breaking it down into manageable steps can make the process less intimidating. This article will outline the 5 easy steps to Blue Cross Blue Shield prior auth, providing clarity and guidance for those seeking to understand and navigate this process effectively.
Understanding Prior Authorization and Blue Cross Blue Shield

Prior authorization is a process used by health insurance companies to determine whether a particular treatment, medication, or service is medically necessary and will be covered under the patient's insurance plan. Blue Cross Blue Shield, being one of the largest health insurance providers, utilizes prior auth to ensure that the care provided to its members is both necessary and cost-effective.
The Importance of Understanding the Prior Auth Process
Understanding the prior auth process is crucial for both healthcare providers and patients. It can significantly impact the timeliness and quality of care received. A clear understanding of the steps involved can help minimize delays, reduce administrative burdens, and ensure that patients receive the necessary treatments without undue complications.
Step 1: Verify Patient Eligibility and Coverage

The first step in the prior auth process is to verify the patient's eligibility and coverage under their BCBS plan. This involves confirming the patient's active status with BCBS, understanding the specifics of their coverage, including any limitations or exclusions, and identifying any requirements for pre-certification or prior authorization.
- Why Verification is Important: Incorrect assumptions about coverage can lead to denied claims and financial burdens on patients.
- How to Verify: Healthcare providers can use BCBS's online portal, mobile app, or contact their customer service directly to verify patient eligibility.
Step 2: Review BCBS Prior Auth Requirements

After verifying the patient's eligibility, the next step is to review BCBS's prior auth requirements for the specific treatment, medication, or service in question. This involves checking BCBS's website, policy documents, or contacting BCBS directly to determine if prior auth is needed and what documentation is required.
- Understanding Requirements: Knowing what is required for prior auth can help streamline the process and prevent unnecessary delays.
- Where to Find Information: BCBS typically publishes prior auth requirements on their website or through provider portals.
Step 3: Gather Necessary Documentation

With the prior auth requirements in hand, the next step is to gather all necessary documentation. This may include clinical notes, lab results, imaging studies, and any other relevant information that supports the medical necessity of the requested treatment or service.
- Why Documentation is Key: Adequate documentation is crucial for a successful prior auth request. It helps BCBS understand the medical necessity of the treatment.
- Tips for Documentation: Ensure all documents are up-to-date, complete, and clearly support the requested treatment.
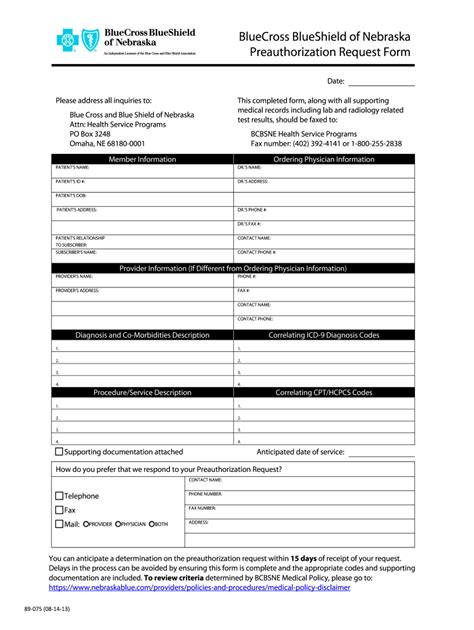
Step 4: Submit the Prior Auth Request

Once all necessary documentation is gathered, the next step is to submit the prior auth request to BCBS. This can typically be done through BCBS's online portal, by fax, or by mail, depending on BCBS's specified submission methods.
- Timing is Everything: Submitting the request in a timely manner is crucial to avoid delays in treatment.
- Follow-up: It's a good idea to follow up with BCBS to ensure the request was received and is being processed.
Step 5: Follow Up and Appeal If Necessary

The final step in the prior auth process is to follow up on the status of the request and to appeal if the request is denied. Following up ensures that the request does not fall through the cracks, and appealing a denial can provide a second chance for approval.
- Navigating Denials: Understanding the reason for denial and addressing those concerns in an appeal can significantly improve the chances of a successful appeal.
- Persistence Pays: Don't be discouraged by initial denials. Persistence and providing additional information can lead to approval.
Final Thoughts
Navigating the prior auth process with Blue Cross Blue Shield requires patience, persistence, and a clear understanding of the steps involved. By following these 5 easy steps, healthcare providers and patients can work together to ensure that necessary treatments and services are approved in a timely manner. Remember, understanding and navigating the prior auth process is key to minimizing delays and ensuring that patients receive the care they need.
What is prior authorization and why is it necessary?
+Prior authorization is a process used by health insurance companies to determine if a particular treatment, medication, or service is medically necessary and covered under the patient's insurance plan. It's necessary to ensure that care is both necessary and cost-effective.
How do I verify a patient's eligibility and coverage with BCBS?
+You can verify a patient's eligibility and coverage by using BCBS's online portal, mobile app, or by contacting their customer service directly.
What if my prior auth request is denied?
+If your prior auth request is denied, you can appeal the decision. Understand the reason for denial and address those concerns in your appeal. Persistence and providing additional information can lead to approval.