Understanding the importance of health insurance predetermination is crucial for patients and healthcare providers alike. A predetermination form is a document that allows patients to receive pre-approval for specific medical treatments or procedures, ensuring that they will be covered by their insurance provider. Blue Cross Blue Shield of Texas (BCBSTX) is one of the largest health insurance providers in the state, and navigating their predetermination form approval process can be daunting. In this article, we will break down the 5 steps to BCBSTX predetermination form approval, providing you with the necessary information to ensure a smooth and successful process.
What is a Predetermination Form?
Before we dive into the approval process, it's essential to understand what a predetermination form is and why it's necessary. A predetermination form is a document that patients or healthcare providers submit to their insurance provider to determine whether a specific medical treatment or procedure will be covered. This form is usually required for non-emergency procedures, such as elective surgeries or high-cost treatments. By submitting a predetermination form, patients can avoid surprise medical bills and ensure that they will be covered for the necessary treatment.

Step 1: Review BCBSTX's Predetermination Policy
The first step in the approval process is to review BCBSTX's predetermination policy. This policy outlines the specific requirements and guidelines for submitting a predetermination form. Patients or healthcare providers can find this information on BCBSTX's website or by contacting their customer service department. It's essential to review the policy carefully to ensure that all necessary information is included in the submission.
Key Components of BCBSTX's Predetermination Policy:
- Eligibility requirements for predetermination
- Required documentation and information
- Submission deadlines and timelines
- Review and approval process

Step 2: Gather Required Documentation and Information
Once you have reviewed BCBSTX's predetermination policy, it's essential to gather all required documentation and information. This may include:
- Patient's medical records and history
- Treatment plan and proposed procedures
- Estimated costs and billing information
- Supporting documentation from healthcare providers
Tips for Gathering Required Documentation:
- Ensure that all documentation is accurate and up-to-date
- Include all relevant medical information and test results
- Use standardized forms and templates to ensure consistency

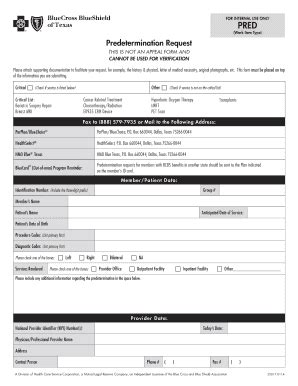
Step 3: Submit the Predetermination Form
With all required documentation and information gathered, it's time to submit the predetermination form. Patients or healthcare providers can submit the form online, by mail, or by fax, depending on BCBSTX's preferred method. It's essential to ensure that the form is complete and accurate to avoid delays or rejection.
Tips for Submitting the Predetermination Form:
- Double-check all information for accuracy and completeness
- Use BCBSTX's online portal or designated submission method
- Keep a record of the submission date and tracking number

Step 4: Review and Respond to BCBSTX's Determination
After submitting the predetermination form, BCBSTX will review the information and make a determination regarding coverage. Patients or healthcare providers will receive a response outlining the decision, which may include approval, denial, or request for additional information.
Understanding BCBSTX's Determination:
- Review the response carefully to understand the decision
- Ensure that all questions and concerns are addressed
- Respond promptly to any requests for additional information

Step 5: Appeal the Determination (If Necessary)
If BCBSTX denies coverage or requests additional information, patients or healthcare providers may need to appeal the determination. This involves submitting additional documentation or information to support the request for coverage.
Tips for Appealing the Determination:
- Review BCBSTX's appeal process carefully
- Gather all necessary documentation and information
- Submit the appeal promptly to avoid delays

By following these 5 steps, patients and healthcare providers can ensure a smooth and successful predetermination form approval process with BCBSTX. Remember to review the policy carefully, gather all required documentation and information, submit the form accurately and completely, review and respond to BCBSTX's determination, and appeal the decision if necessary.
Take Action:
We hope this article has provided you with the necessary information to navigate the BCBSTX predetermination form approval process successfully. If you have any questions or concerns, please don't hesitate to comment below or share this article with others who may benefit from this information. Remember to stay informed and take control of your healthcare by understanding the importance of predetermination forms.
What is a predetermination form?
+A predetermination form is a document that patients or healthcare providers submit to their insurance provider to determine whether a specific medical treatment or procedure will be covered.
Why is a predetermination form necessary?
+A predetermination form is necessary to avoid surprise medical bills and ensure that patients will be covered for the necessary treatment.
How do I submit a predetermination form to BCBSTX?
+Patient's or healthcare providers can submit the form online, by mail, or by fax, depending on BCBSTX's preferred method.