The daunting task of navigating the complex world of health insurance appeals can be overwhelming, especially when it comes to completing the BCBSNC appeal form. Blue Cross Blue Shield of North Carolina (BCBSNC) is a prominent health insurance provider, and understanding the appeal process is crucial for policyholders who have had a claim denied or partially denied. In this article, we will break down the BCBSNC appeal form into manageable steps, providing you with the knowledge and confidence to successfully complete the process.
Understanding the BCBSNC Appeal Process
Before diving into the steps, it's essential to comprehend the BCBSNC appeal process. An appeal is a formal request to review a decision made by BCBSNC regarding a claim or coverage. This process is designed to ensure that policyholders receive fair and accurate decisions. BCBSNC allows policyholders to appeal decisions within a specified timeframe, usually 180 days from the date of the initial decision.

Step 1: Review and Understand the Denial Letter
The first step in completing the BCBSNC appeal form is to thoroughly review the denial letter sent by BCBSNC. This letter will outline the reason for the denial, the specific policy provisions that apply, and instructions on how to appeal the decision. It's crucial to understand the reason for the denial, as this will help you prepare a strong appeal.
- Take note of the specific policy provisions cited in the denial letter.
- Identify the key points that led to the denial decision.
- Gather all relevant documentation, including medical records and billing statements.
Step 2: Gather Supporting Documentation
To build a strong appeal, it's essential to gather supporting documentation that addresses the reason for the denial. This may include:
-
Medical records that demonstrate the medical necessity of the treatment or service.
-
Billing statements that show the correct coding and billing information.
-
Letters from healthcare providers that explain the treatment or service.
-
Any other relevant documentation that supports your appeal.
-
Organize your documentation in a clear and concise manner.
-
Ensure that all documentation is up-to-date and relevant to the appeal.
-
Make sure to keep a copy of all documentation for your records.

Step 3: Complete the BCBSNC Appeal Form
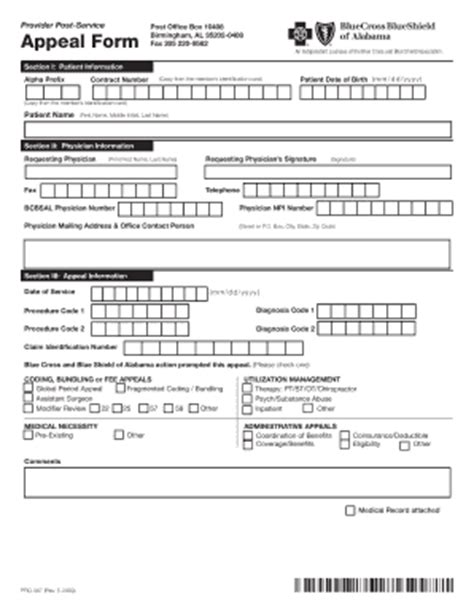
The BCBSNC appeal form is a critical component of the appeal process. The form will ask for specific information, including:
-
Policyholder information, including name, address, and policy number.
-
Claim information, including claim number and date of service.
-
A detailed explanation of the reason for the appeal.
-
Supporting documentation, as gathered in Step 2.
-
Complete the form accurately and thoroughly.
-
Ensure that all required fields are filled in.
-
Attach all supporting documentation to the form.
Step 4: Submit the Appeal Form
Once the appeal form is complete, it's time to submit it to BCBSNC. There are several ways to submit the form, including:
-
Mail: Send the form and supporting documentation to the address listed on the form.
-
Fax: Fax the form and supporting documentation to the number listed on the form.
-
Online: Submit the form and supporting documentation through the BCBSNC website.
-
Ensure that the form is submitted within the specified timeframe (usually 180 days).
-
Keep a copy of the submitted form and documentation for your records.

Step 5: Follow Up on the Appeal Status
After submitting the appeal form, it's essential to follow up on the appeal status. BCBSNC will review the appeal and make a determination within a specified timeframe (usually 30-60 days). You can check the status of your appeal by:
-
Calling the BCBSNC customer service number.
-
Logging into your online account.
-
Checking your email for updates.
-
Follow up on the appeal status regularly to ensure that it is being processed.
-
Be prepared to provide additional information or documentation, if requested.
By following these 5 steps, you can successfully complete the BCBSNC appeal form and navigate the appeal process with confidence. Remember to stay organized, gather supporting documentation, and follow up on the appeal status to ensure a smooth and efficient process.

We encourage you to share your experiences with the BCBSNC appeal form in the comments below. Have you successfully completed the appeal process? What tips and advice can you offer to others navigating this process? Share your thoughts and help others achieve a successful outcome.
What is the BCBSNC appeal form?
+The BCBSNC appeal form is a document used to formally request a review of a denied claim or coverage decision made by Blue Cross Blue Shield of North Carolina.
How long do I have to submit an appeal?
+Policyholders typically have 180 days from the date of the initial decision to submit an appeal.
What documentation do I need to support my appeal?
+Supporting documentation may include medical records, billing statements, letters from healthcare providers, and any other relevant documentation that supports your appeal.