The healthcare landscape is complex, and navigating the nuances of insurance coverage can be a daunting task for both patients and healthcare providers. One aspect of this landscape is the prior authorization process, which can be particularly challenging. For those seeking medical care in Oklahoma, understanding the BCBS Oklahoma prior authorization form is crucial. In this article, we will delve into the details of this form, explore its importance, and provide guidance on how to navigate the process with ease.
Healthcare providers and patients alike must contend with the administrative tasks associated with seeking medical care. Among these tasks, prior authorization stands out as a critical step that can significantly impact the delivery of care. Prior authorization is a process where a healthcare provider must obtain approval from a patient's insurance provider before administering certain treatments or medications. This process aims to ensure that the proposed treatment is medically necessary and aligns with the insurance coverage.

Understanding the BCBS Oklahoma Prior Authorization Form
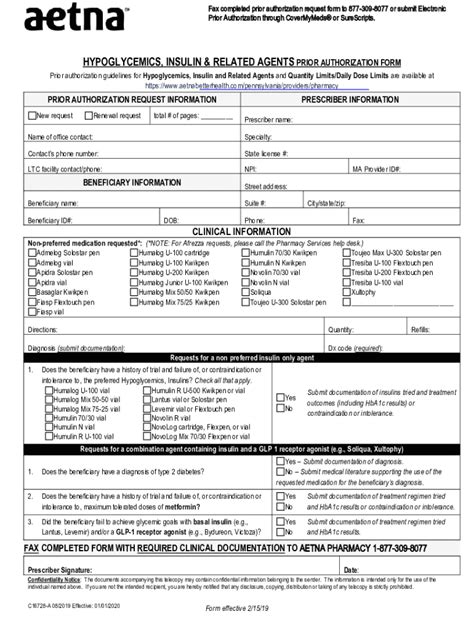
The BCBS Oklahoma prior authorization form is a critical document that healthcare providers must complete and submit to Blue Cross Blue Shield of Oklahoma (BCBSOK) to request approval for specific medical treatments or services. This form serves as a gateway to accessing necessary care, and its accurate completion is vital for a successful outcome.
Why Is the BCBS Oklahoma Prior Authorization Form Important?
The BCBS Oklahoma prior authorization form is essential for several reasons:
• Ensures Medical Necessity: It helps verify that the requested treatment or service is medically necessary and aligns with established medical guidelines. • Prevents Denials: Proper completion of the form reduces the likelihood of authorization denials, which can delay or prevent access to care. • Streamlines the Process: A well-documented form expedites the review process, enabling BCBSOK to make informed decisions more efficiently.
Navigating the BCBS Oklahoma Prior Authorization Process
While the prior authorization process can seem daunting, understanding the steps involved can make it more manageable. Here's a simplified overview of the process:

- Determine If Prior Authorization Is Required: Check the BCBSOK website or consult with the patient's insurance plan documents to determine if prior authorization is needed for the specific treatment or service.
- Gather Necessary Information: Collect relevant medical records, test results, and any other documentation that supports the medical necessity of the requested treatment.
- Complete the Prior Authorization Form: Fill out the BCBS Oklahoma prior authorization form accurately and thoroughly, ensuring all required information is included.
- Submit the Form: Send the completed form to BCBSOK via fax, mail, or online submission, depending on the preferred method.
- Follow Up: After submitting the form, follow up with BCBSOK to confirm receipt and to inquire about the status of the authorization request.
Tips for a Smooth Prior Authorization Process
To ensure a smooth and efficient prior authorization process:
• Verify Patient Eligibility: Confirm the patient's insurance coverage and eligibility before submitting the prior authorization request. • Provide Complete Information: Ensure the prior authorization form is thoroughly completed, and all supporting documentation is included. • Submit Requests Electronically: Utilize online submission or faxing to expedite the process and reduce errors. • Follow Up Regularly: Regularly check on the status of the authorization request to prevent delays.
Benefits of Electronic Prior Authorization
In recent years, electronic prior authorization (ePA) has gained popularity as a more efficient and streamlined approach to the traditional paper-based process. The benefits of ePA include:

• Reduced Administrative Burden: ePA automates the process, reducing manual labor and minimizing errors. • Increased Efficiency: Electronic submissions expedite the review process, enabling faster decision-making. • Improved Patient Outcomes: By streamlining the process, ePA helps ensure patients receive necessary treatments more promptly.
Common Challenges in the Prior Authorization Process
Despite the benefits of prior authorization, challenges persist:
• Delays in Care: Lengthy review processes can delay access to necessary treatments. • Administrative Burden: Manual submission and tracking of prior authorization requests can be time-consuming. • Denials and Appeals: Inaccurate or incomplete submissions can lead to denials, requiring appeals and further delays.
Conclusion - A Simplified Approach to BCBS Oklahoma Prior Authorization
Navigating the BCBS Oklahoma prior authorization form and process can be complex, but by understanding the importance of this process and following the outlined steps, healthcare providers and patients can work together to ensure seamless access to necessary care. By embracing electronic prior authorization and adhering to best practices, the administrative burden can be reduced, and patient outcomes can be improved.

If you have any questions or need assistance with the BCBS Oklahoma prior authorization form, please don't hesitate to comment below or share this article with others who may benefit from this information.
What is the purpose of the BCBS Oklahoma prior authorization form?
+The BCBS Oklahoma prior authorization form is used to request approval for specific medical treatments or services, ensuring that the proposed treatment is medically necessary and aligns with the insurance coverage.
How do I submit the BCBS Oklahoma prior authorization form?
+The form can be submitted via fax, mail, or online submission, depending on the preferred method.
What are the benefits of electronic prior authorization?
+Electronic prior authorization (ePA) offers several benefits, including reduced administrative burden, increased efficiency, and improved patient outcomes.