The healthcare industry is a complex and multifaceted sector that requires a high level of administrative efficiency to ensure smooth operations. One crucial aspect of this is the claim review process, which helps healthcare providers and insurance companies verify the accuracy and legitimacy of medical claims. In Texas, the Blue Cross Blue Shield (BCBS) of Texas plays a significant role in providing health insurance coverage to millions of people. To facilitate the claim review process, BCBS of Texas has a standardized claim review form that healthcare providers must use when submitting claims for review.
The importance of accurate and efficient claim review cannot be overstated. For healthcare providers, a smooth claim review process means reduced administrative burdens and faster reimbursement for services rendered. For insurance companies like BCBS of Texas, accurate claim review helps minimize errors and prevent unnecessary payouts. In this article, we will delve into the world of BCBS of Texas claim review forms, exploring the benefits, the process, and best practices for healthcare providers.
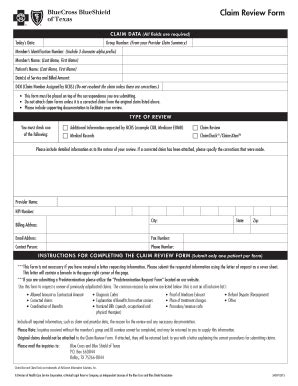
Understanding the BCBS of Texas Claim Review Form

The BCBS of Texas claim review form is a standardized document designed to gather essential information about medical claims submitted by healthcare providers. The form typically includes fields for:
- Patient demographics and insurance information
- Claim details, including dates of service and procedure codes
- Supporting documentation, such as medical records and invoices
By using this standardized form, healthcare providers can ensure that their claims are complete and accurate, reducing the likelihood of delays or rejections.
Benefits of the BCBS of Texas Claim Review Form
The BCBS of Texas claim review form offers several benefits to healthcare providers and insurance companies alike. Some of the key advantages include:
- Improved accuracy: By using a standardized form, healthcare providers can reduce errors and ensure that their claims are complete and accurate.
- Increased efficiency: The claim review form streamlines the review process, allowing insurance companies to quickly and easily verify the information provided.
- Faster reimbursement: By reducing errors and delays, healthcare providers can expect faster reimbursement for their services.
- Better communication: The claim review form provides a clear and concise way for healthcare providers to communicate with insurance companies, reducing misunderstandings and miscommunications.
The Claim Review Process: A Step-by-Step Guide

The claim review process involves several steps, from submission to final determination. Here's a step-by-step guide to help healthcare providers navigate the process:
- Submission: Healthcare providers submit the completed claim review form, along with supporting documentation, to BCBS of Texas.
- Initial Review: BCBS of Texas reviews the claim to ensure that it is complete and accurate.
- Verification: BCBS of Texas verifies the information provided, including patient demographics, claim details, and supporting documentation.
- Determination: BCBS of Texas makes a determination on the claim, either approving or denying payment.
- Notification: BCBS of Texas notifies the healthcare provider of the determination, along with any additional information or requests for further documentation.
Best Practices for Healthcare Providers
To ensure a smooth claim review process, healthcare providers can follow these best practices:
- Use the standardized claim review form to ensure accuracy and completeness.
- Submit claims in a timely manner to avoid delays.
- Provide clear and concise documentation to support the claim.
- Respond promptly to requests for additional information or documentation.
- Keep accurate records of all correspondence and documentation related to the claim.
Common Mistakes to Avoid

While the claim review process can be complex, there are several common mistakes that healthcare providers can avoid:
- Incomplete or inaccurate information on the claim review form.
- Failure to submit supporting documentation.
- Delays in responding to requests for additional information or documentation.
- Inadequate records of correspondence and documentation related to the claim.
By avoiding these common mistakes, healthcare providers can reduce errors and delays, ensuring a smoother claim review process.
Conclusion
The BCBS of Texas claim review form is an essential tool for healthcare providers and insurance companies alike. By understanding the benefits and process of the claim review form, healthcare providers can ensure accurate and efficient submission of claims, reducing administrative burdens and improving reimbursement. By following best practices and avoiding common mistakes, healthcare providers can navigate the claim review process with confidence.
We invite you to share your thoughts and experiences with the BCBS of Texas claim review form in the comments section below. Your feedback can help healthcare providers and insurance companies improve the claim review process, ensuring better outcomes for patients and providers alike.
What is the purpose of the BCBS of Texas claim review form?
+The BCBS of Texas claim review form is a standardized document designed to gather essential information about medical claims submitted by healthcare providers.
What are the benefits of using the BCBS of Texas claim review form?
+The benefits of using the BCBS of Texas claim review form include improved accuracy, increased efficiency, faster reimbursement, and better communication between healthcare providers and insurance companies.
What are some common mistakes to avoid when submitting a claim review form?
+Common mistakes to avoid include incomplete or inaccurate information on the claim review form, failure to submit supporting documentation, delays in responding to requests for additional information or documentation, and inadequate records of correspondence and documentation related to the claim.