In the vast landscape of health insurance, navigating the intricacies of pre-service coverage reviews can be daunting for both patients and healthcare providers. One essential tool in this process is the BCBS of Texas predetermination form, used by Blue Cross Blue Shield of Texas (BCBSTX) to assess the medical necessity of a proposed treatment or service. This article will delve into the world of BCBS of Texas predetermination, explaining its purpose, the process of submitting a request, and the benefits of utilizing this form.
Understanding the BCBS of Texas Predetermination Form

The BCBS of Texas predetermination form is a crucial document that facilitates communication between healthcare providers, patients, and BCBSTX regarding the coverage of proposed medical services. By submitting this form, providers can obtain a predetermination of benefits, which is essentially an estimate of the patient's coverage for a specific treatment or service. This process helps in managing patient expectations and financial responsibilities upfront, reducing the likelihood of unexpected medical bills.
The Importance of Predetermination
Predetermination plays a vital role in the healthcare system by ensuring that patients receive necessary care while also managing costs. It helps providers to:
- Verify the patient's coverage for the proposed treatment.
- Understand the patient's out-of-pocket expenses.
- Identify any potential coverage issues early on.
- Plan for alternative treatments if necessary.
The Process of Submitting a BCBS of Texas Predetermination Form

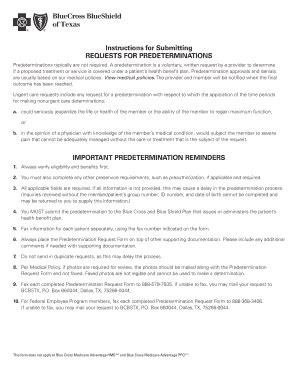
The process of submitting a BCBS of Texas predetermination form involves several steps:
-
Gather Information: The healthcare provider must collect all relevant information about the patient's condition, the proposed treatment, and the patient's insurance plan details.
-
Fill Out the Form: The provider fills out the BCBS of Texas predetermination form accurately, ensuring all required fields are completed. This includes patient demographics, procedure codes, and detailed descriptions of the proposed services.
-
Submit the Form: The completed form is then submitted to BCBSTX. This can typically be done electronically or by mail, depending on the preference of the provider and the requirements of BCBSTX.
-
Review and Determination: BCBSTX reviews the submitted form to assess the medical necessity of the proposed treatment. They may request additional information or clarification during this process.
-
Notification: Once the review is complete, BCBSTX notifies the provider of their determination. This notification includes details of the estimated benefits coverage for the proposed services.
Tips for a Smooth Predetermination Process
- Accuracy is Key: Ensure that all information on the form is accurate and up-to-date.
- Include All Necessary Documents: Supporting documents, such as medical records and test results, should be included with the submission.
- Plan Ahead: Submit the form well in advance of the proposed treatment date to allow time for the review process.
Benefits of Using the BCBS of Texas Predetermination Form

The use of the BCBS of Texas predetermination form offers several benefits for both patients and healthcare providers, including:
- Financial Clarity: Patients gain a clear understanding of their financial responsibilities before undergoing treatment.
- Reduced Surprise Billing: The risk of unexpected medical bills is significantly reduced.
- Streamlined Care: Providers can plan care more effectively, knowing in advance what services are covered.
- Enhanced Patient Satisfaction: By managing expectations and reducing financial stress, patient satisfaction with care is enhanced.
Conclusion - Navigating the Path Forward

In conclusion, the BCBS of Texas predetermination form is a valuable tool in the healthcare landscape, offering clarity and transparency in the coverage of proposed medical services. By understanding the purpose, process, and benefits of this form, healthcare providers can navigate the complexities of insurance coverage with ease, ultimately enhancing the patient care experience.
If you have found this information helpful or have further questions about the BCBS of Texas predetermination form, we encourage you to share your thoughts in the comments section. Your input is invaluable in creating a community that understands and navigates the intricacies of health insurance with confidence.
What is the primary purpose of the BCBS of Texas predetermination form?
+The primary purpose of the BCBS of Texas predetermination form is to obtain an estimate of the patient's coverage for a specific medical treatment or service before it is provided.
How does the predetermination process benefit patients?
+The predetermination process benefits patients by providing clarity on their financial responsibilities for the proposed treatment, reducing the risk of surprise medical bills, and enhancing overall patient satisfaction.
What information is required to fill out the BCBS of Texas predetermination form?
+To fill out the form, healthcare providers need to gather information about the patient's demographics, the proposed treatment details (including procedure codes), and the patient's insurance plan details.