Prior authorization is a crucial step in the healthcare process, ensuring that patients receive necessary treatments while minimizing unnecessary costs. For those dealing with BCBS Michigan, navigating the prior authorization process can be daunting. However, with the right guidance, it can be done efficiently. Here's a step-by-step guide on how to handle BCBS Michigan prior authorization via fax, making the process smoother for healthcare providers and patients alike.
Understanding Prior Authorization
Prior authorization, also known as pre-authorization, is a process used by health insurance companies to determine whether they will cover a prescribed procedure, service, or medication. It's essentially a way to ensure that the treatment is medically necessary and aligns with the insurance policy's coverage. BCBS Michigan, like many other insurance providers, requires prior authorization for certain medical services to ensure that the patient receives the most appropriate and cost-effective care.
Benefits of Prior Authorization
While the prior authorization process might seem like an additional hurdle, it has several benefits:
- Ensures that patients receive medically necessary treatments.
- Helps in reducing healthcare costs by avoiding unnecessary procedures.
- Encourages the use of generic or cost-effective alternatives when possible.
- Facilitates better communication between healthcare providers, patients, and insurance companies.
Step 1: Gather Necessary Information
Before initiating the prior authorization process, it's essential to gather all the necessary information. This typically includes:
- Patient's insurance details (policy number, group number, etc.)
- Description of the treatment, service, or medication requiring authorization
- Medical necessity documentation (e.g., test results, diagnosis, etc.)
- Healthcare provider's information (name, contact details, NPI, etc.)

Step 2: Check BCBS Michigan's Prior Authorization Requirements
BCBS Michigan has specific requirements and guidelines for prior authorization. Healthcare providers should:
- Visit the BCBS Michigan website to review their prior authorization policy.
- Check if the specific treatment or medication requires authorization.
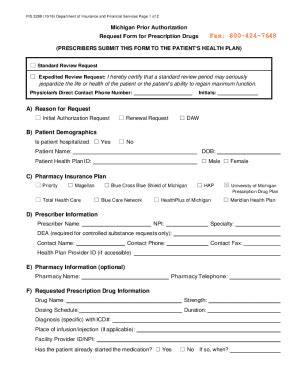
- Download and fill out the appropriate prior authorization form.
Step 3: Fill Out the Prior Authorization Form
Once you've obtained the correct form, fill it out completely and accurately. Ensure that all required fields are filled in, and all necessary documentation is attached. Incomplete forms can lead to delays or even denial of authorization.
Step 4: Fax the Prior Authorization Request
After completing the form and gathering all necessary documents, fax the prior authorization request to BCBS Michigan. The fax number can be found on the BCBS Michigan website or on the prior authorization form. It's crucial to keep a record of the fax transmission for future reference.

Step 5: Follow Up on the Prior Authorization Status
After submitting the prior authorization request, it's essential to follow up on its status. BCBS Michigan typically processes these requests within a few days, but the exact timeframe may vary. Healthcare providers can check the status online or by contacting BCBS Michigan directly.
Tips for a Smooth Prior Authorization Process
- Ensure all forms are filled out correctly and completely.
- Attach all necessary documentation to avoid delays.
- Keep a record of the fax transmission and any communication with BCBS Michigan.
- Follow up promptly on the status of the prior authorization request.
By following these steps and tips, healthcare providers can navigate the BCBS Michigan prior authorization process via fax efficiently. Remember, prior authorization is a critical step in ensuring that patients receive necessary care while managing healthcare costs.
Navigating the Future of Prior Authorization
As healthcare continues to evolve, the prior authorization process may undergo changes, incorporating more technology and automation. Staying informed about these developments and adapting to new guidelines will be key to ensuring a seamless patient care experience.

Conclusion
In conclusion, navigating the BCBS Michigan prior authorization process via fax requires attention to detail and a clear understanding of the process. By following the steps outlined above and staying informed about any updates or changes, healthcare providers can ensure that their patients receive the necessary care while minimizing delays and complications. Remember, effective communication and proactive follow-up are key to a successful prior authorization process.

Share Your Thoughts
Have you experienced the BCBS Michigan prior authorization process? Share your insights, tips, or challenges in the comments below. Your input can help other healthcare providers navigate this process more effectively.
What is prior authorization?
+Prior authorization, also known as pre-authorization, is a process used by health insurance companies to determine whether they will cover a prescribed procedure, service, or medication.
Why is prior authorization required?
+Prior authorization ensures that patients receive medically necessary treatments and helps in reducing healthcare costs by avoiding unnecessary procedures.
How long does the prior authorization process take?
+The exact timeframe may vary, but BCBS Michigan typically processes prior authorization requests within a few days.