Understanding BCBS FEP Pharmacy Prior Authorization Form Requirements

Pharmacy prior authorization forms are a crucial part of the healthcare system, ensuring that patients receive the medications they need while controlling costs. For federal employees, retirees, and their families, the Blue Cross Blue Shield Federal Employee Program (BCBS FEP) provides comprehensive health insurance coverage, including pharmacy benefits. In this article, we'll delve into the BCBS FEP pharmacy prior authorization form requirements, explaining the process, benefits, and necessary steps for healthcare providers and patients.
What is Prior Authorization, and Why is it Necessary?

Prior authorization is a process used by health insurance companies to determine whether a specific medication or treatment is medically necessary and covered under the patient's insurance plan. This process helps ensure that patients receive safe and effective treatments while minimizing unnecessary costs. In the context of BCBS FEP, prior authorization is required for certain medications, including specialty medications, injectables, and high-cost medications.
Benefits of Prior Authorization
Prior authorization offers several benefits to patients, healthcare providers, and insurance companies:
- Ensures patient safety by verifying the medical necessity of medications
- Helps control healthcare costs by minimizing unnecessary prescriptions
- Encourages the use of cost-effective medications and treatments
- Enhances patient outcomes by ensuring that medications are used appropriately
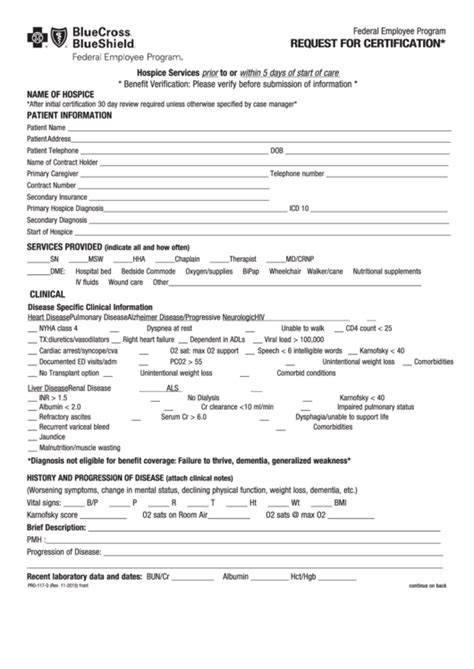
BCBS FEP Pharmacy Prior Authorization Form Requirements

To initiate the prior authorization process, healthcare providers must submit a completed prior authorization form to BCBS FEP. The form requires the following information:
- Patient demographics and insurance information
- Medication name, dosage, and frequency
- Diagnosis or medical condition being treated
- Medical justification for the medication
- Supporting clinical documentation (e.g., lab results, medical records)
Steps for Submitting a Prior Authorization Request
To ensure a smooth prior authorization process, follow these steps:
- Verify patient eligibility: Confirm that the patient is eligible for BCBS FEP coverage and has an active pharmacy benefit.
- Complete the prior authorization form: Fill out the prior authorization form in its entirety, ensuring that all required information is provided.
- Submit supporting documentation: Include relevant clinical documentation to support the prior authorization request.
- Submit the request: Fax or mail the completed prior authorization form and supporting documentation to BCBS FEP.
- Follow up: If necessary, follow up with BCBS FEP to confirm receipt of the prior authorization request and to obtain a determination.
What to Expect After Submitting a Prior Authorization Request

After submitting a prior authorization request, BCBS FEP will review the information and make a determination. This process typically takes 1-3 business days, but may take longer in certain circumstances.
- Approved: If the prior authorization request is approved, the patient's medication will be covered under their insurance plan.
- Denied: If the prior authorization request is denied, the patient's medication will not be covered under their insurance plan. In this case, the patient or healthcare provider may appeal the decision.
- Additional information required: If BCBS FEP requires additional information to make a determination, the patient or healthcare provider will be notified.
Common Reasons for Prior Authorization Denials

Prior authorization requests may be denied for various reasons, including:
- Lack of medical necessity: The requested medication is not medically necessary for the patient's condition.
- Insufficient documentation: The prior authorization form or supporting documentation is incomplete or inadequate.
- Non-covered medication: The requested medication is not covered under the patient's insurance plan.
- Alternative therapies available: Alternative treatments or medications are available that are more cost-effective or clinically effective.
Appealing a Prior Authorization Denial

If a prior authorization request is denied, the patient or healthcare provider may appeal the decision. To appeal, follow these steps:
- Review the denial letter: Understand the reason for the denial and the required next steps.
- Gather additional information: Collect any additional information or documentation required to support the appeal.
- Submit the appeal: Fax or mail the appeal request and supporting documentation to BCBS FEP.
- Follow up: If necessary, follow up with BCBS FEP to confirm receipt of the appeal request and to obtain a determination.
In conclusion, understanding the BCBS FEP pharmacy prior authorization form requirements is crucial for healthcare providers and patients. By following the steps outlined in this article, you can ensure a smooth prior authorization process and help patients receive the medications they need.
We encourage you to share your experiences or ask questions about the BCBS FEP pharmacy prior authorization process in the comments below.
What is the purpose of prior authorization?
+Prior authorization is a process used by health insurance companies to determine whether a specific medication or treatment is medically necessary and covered under the patient's insurance plan.
What information is required on the BCBS FEP pharmacy prior authorization form?
+The form requires patient demographics and insurance information, medication name, dosage, and frequency, diagnosis or medical condition being treated, medical justification for the medication, and supporting clinical documentation.
How long does the prior authorization process typically take?
+The prior authorization process typically takes 1-3 business days, but may take longer in certain circumstances.