Understanding the BCBS Federal Prior Authorization Form: A Comprehensive Guide

Prior authorization is a critical step in the healthcare process, ensuring that patients receive necessary medical treatments while also controlling healthcare costs. Blue Cross Blue Shield (BCBS) Federal, a leading healthcare provider, has implemented a prior authorization form to streamline this process. In this article, we will delve into the BCBS Federal Prior Authorization Form, exploring its purpose, benefits, and step-by-step guide on how to complete it.
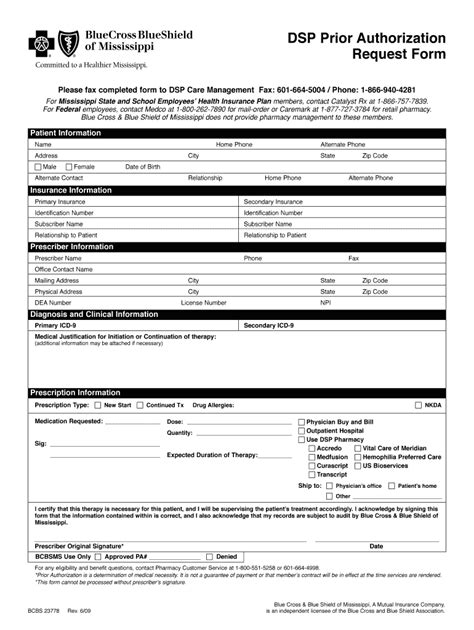
What is the BCBS Federal Prior Authorization Form?
The BCBS Federal Prior Authorization Form is a document used by healthcare providers to request prior authorization for medical treatments, services, or medications for their patients. This form is designed to ensure that patients receive necessary medical care while also controlling healthcare costs by verifying the medical necessity of the requested treatment.
Benefits of the BCBS Federal Prior Authorization Form

The BCBS Federal Prior Authorization Form offers several benefits to both healthcare providers and patients. Some of the key benefits include:
- Improved Patient Care: By verifying the medical necessity of treatments, the prior authorization form ensures that patients receive necessary medical care, reducing the risk of adverse reactions or complications.
- Reduced Healthcare Costs: The prior authorization form helps control healthcare costs by eliminating unnecessary treatments and services.
- Streamlined Process: The form simplifies the prior authorization process, reducing the administrative burden on healthcare providers and patients.
- Increased Transparency: The form provides a clear and transparent process for prior authorization, reducing the risk of errors or misunderstandings.
Step-by-Step Guide to Completing the BCBS Federal Prior Authorization Form
Completing the BCBS Federal Prior Authorization Form is a straightforward process that requires careful attention to detail. Here is a step-by-step guide to help healthcare providers complete the form:
- Patient Information: Enter the patient's name, date of birth, and member ID number.
- Provider Information: Enter the healthcare provider's name, address, and contact information.
- Treatment Information: Describe the treatment or service being requested, including the diagnosis, procedure code, and medication (if applicable).
- Medical Necessity: Explain the medical necessity of the treatment or service, including the patient's medical history and any relevant test results.
- Supporting Documentation: Attach any supporting documentation, such as test results, medical records, or medication lists.
- Signature: Sign and date the form, certifying that the information provided is accurate and complete.
Common Mistakes to Avoid When Completing the BCBS Federal Prior Authorization Form

When completing the BCBS Federal Prior Authorization Form, it is essential to avoid common mistakes that can delay or deny prior authorization. Some common mistakes to avoid include:
- Incomplete or Inaccurate Information: Ensure that all required fields are completed accurately and thoroughly.
- Lack of Supporting Documentation: Attach all required supporting documentation to avoid delays or denials.
- Insufficient Medical Necessity: Clearly explain the medical necessity of the treatment or service to avoid denials.
FAQs About the BCBS Federal Prior Authorization Form
What is the purpose of the BCBS Federal Prior Authorization Form?
+The BCBS Federal Prior Authorization Form is used to request prior authorization for medical treatments, services, or medications, ensuring that patients receive necessary medical care while controlling healthcare costs.
How do I complete the BCBS Federal Prior Authorization Form?
+Follow the step-by-step guide outlined in this article, ensuring that all required fields are completed accurately and thoroughly, and attach all required supporting documentation.
What are common mistakes to avoid when completing the BCBS Federal Prior Authorization Form?
+Avoid incomplete or inaccurate information, lack of supporting documentation, and insufficient medical necessity, as these can delay or deny prior authorization.
In conclusion, the BCBS Federal Prior Authorization Form is a critical tool in the healthcare process, ensuring that patients receive necessary medical care while controlling healthcare costs. By understanding the form's purpose, benefits, and step-by-step guide, healthcare providers can ensure a smooth and efficient prior authorization process. We encourage you to share your thoughts and experiences with the BCBS Federal Prior Authorization Form in the comments section below.