As healthcare providers and patients navigate the complexities of medical billing and insurance claims, prior authorization has become a crucial step in ensuring that necessary treatments and services are covered by insurance providers. Ascension, a leading healthcare organization, has implemented a prior authorization process to streamline this step and reduce administrative burdens. In this article, we will delve into the Ascension Complete Prior Authorization Form, exploring its purpose, benefits, and simplified process.
What is Prior Authorization?
Prior authorization, also known as pre-authorization or pre-certification, is the process by which healthcare providers obtain approval from insurance providers before administering specific treatments, services, or medications. This step is designed to ensure that patients receive necessary care while minimizing unnecessary costs and ensuring that treatments are medically necessary.

The Importance of Prior Authorization
Prior authorization plays a vital role in the healthcare ecosystem, as it:
- Ensures that patients receive necessary care while minimizing unnecessary costs
- Reduces administrative burdens on healthcare providers
- Helps to prevent denied claims and delayed payments
- Enhances patient safety by verifying the medical necessity of treatments
Ascension Complete Prior Authorization Form: Simplified Process
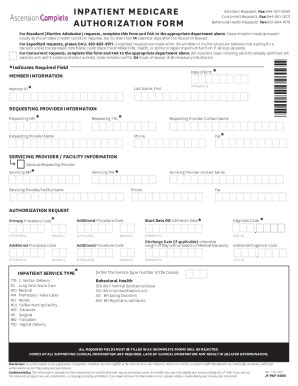
Ascension's prior authorization process is designed to be efficient, straightforward, and patient-centered. The Ascension Complete Prior Authorization Form is a critical component of this process, as it provides a standardized and streamlined way for healthcare providers to request prior authorization.

Benefits of the Ascension Complete Prior Authorization Form
The Ascension Complete Prior Authorization Form offers numerous benefits, including:
- Streamlined process: The form provides a clear and concise way for healthcare providers to request prior authorization, reducing administrative burdens and minimizing delays.
- Improved accuracy: The standardized form ensures that all necessary information is captured, reducing errors and denied claims.
- Enhanced patient experience: By streamlining the prior authorization process, patients can receive necessary care more quickly, reducing wait times and improving health outcomes.
How to Complete the Ascension Complete Prior Authorization Form
To complete the Ascension Complete Prior Authorization Form, healthcare providers should follow these steps:
- Gather necessary information: Ensure that all required patient and treatment information is available, including medical records, test results, and treatment plans.
- Complete the form: Fill out the form accurately and thoroughly, ensuring that all required fields are completed.
- Submit the form: Submit the completed form to Ascension's prior authorization department, either electronically or via fax.
Tips for Healthcare Providers
To ensure a smooth prior authorization process, healthcare providers should:
- Verify patient eligibility: Confirm patient insurance coverage and eligibility before submitting the prior authorization form.
- Use clear and concise language: Ensure that all information on the form is accurate and easily understood.
- Submit complete information: Provide all necessary documentation and information to avoid delays or denied claims.
Patient FAQs
Here are some frequently asked questions from patients regarding the prior authorization process:
What is prior authorization?
+Prior authorization is the process by which healthcare providers obtain approval from insurance providers before administering specific treatments, services, or medications.
Why is prior authorization necessary?
+Prior authorization ensures that patients receive necessary care while minimizing unnecessary costs and ensuring that treatments are medically necessary.
How long does the prior authorization process take?
+The prior authorization process typically takes 24-48 hours, but may vary depending on the complexity of the request and the insurance provider's review process.
By understanding the Ascension Complete Prior Authorization Form and its simplified process, healthcare providers can reduce administrative burdens, improve patient outcomes, and enhance the overall healthcare experience. As the healthcare landscape continues to evolve, streamlined prior authorization processes like Ascension's will play a critical role in ensuring that patients receive necessary care while minimizing unnecessary costs.