The Archimedes Rx Prior Authorization Form is a crucial document that healthcare providers need to complete to ensure that patients receive the necessary medication. The prior authorization process can be complex and time-consuming, but breaking it down into manageable steps can make it more efficient. Here's a step-by-step guide to help you navigate the Archimedes Rx Prior Authorization Form.

Understanding the Archimedes Rx Prior Authorization Form
Before we dive into the steps, it's essential to understand the purpose of the Archimedes Rx Prior Authorization Form. This form is used to request prior authorization for prescription medications that require approval from the patient's insurance provider. The form collects information about the patient, the prescribed medication, and the healthcare provider.
Benefits of Prior Authorization
Prior authorization is a process that ensures patients receive the most effective and cost-efficient treatment. It helps to:
- Reduce healthcare costs by avoiding unnecessary or ineffective treatments
- Improve patient outcomes by ensuring that patients receive the most appropriate medication
- Enhance patient safety by minimizing the risk of adverse reactions or interactions
Step 1: Gather Required Information
Before starting the prior authorization process, you'll need to gather the required information. This includes:
- Patient demographics, such as name, date of birth, and insurance provider
- Prescription information, including the medication name, dosage, and frequency
- Healthcare provider information, including name, contact details, and medical license number
- Clinical information, such as the patient's medical history and diagnosis

Step 2: Complete the Archimedes Rx Prior Authorization Form
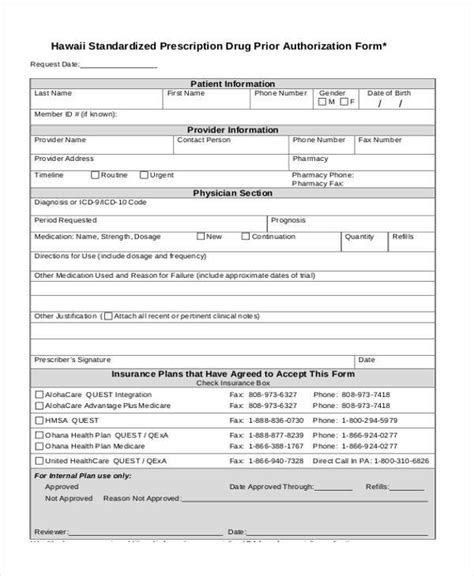
Once you have all the required information, you can start completing the Archimedes Rx Prior Authorization Form. The form typically includes sections for:
- Patient information
- Prescription information
- Healthcare provider information
- Clinical information
- Supporting documentation, such as medical records or test results
Make sure to fill out the form accurately and completely, as incomplete or inaccurate information can delay the prior authorization process.

Step 3: Submit the Archimedes Rx Prior Authorization Form
After completing the form, you'll need to submit it to the patient's insurance provider. This can usually be done online, by fax, or by mail. Make sure to follow the insurance provider's specific submission guidelines to ensure that the form is processed quickly and efficiently.
Submission Methods
- Online submission: Many insurance providers offer online portals for submitting prior authorization forms. This is usually the fastest and most convenient method.
- Fax submission: You can also submit the form by fax, but make sure to use a secure fax line to protect patient confidentiality.
- Mail submission: Mailing the form is the slowest method, but it's still an option for those who prefer it.

Step 4: Follow Up on the Prior Authorization Request
After submitting the Archimedes Rx Prior Authorization Form, it's essential to follow up on the request. This ensures that the form is being processed and that any issues are addressed promptly.
- Follow up with the insurance provider: Contact the insurance provider to confirm that they received the form and to ask about the status of the prior authorization request.
- Check the online portal: If you submitted the form online, you can check the status of the request through the insurance provider's online portal.

Step 5: Receive and Review the Prior Authorization Decision
Once the insurance provider has processed the prior authorization request, they will send a decision to the healthcare provider. This decision will indicate whether the medication is approved or denied.
- Review the decision: Carefully review the decision to ensure that it's accurate and complete.
- Take action: If the medication is approved, you can proceed with filling the prescription. If it's denied, you may need to appeal the decision or consider alternative treatments.

Final Thoughts
The Archimedes Rx Prior Authorization Form is a critical document that helps ensure patients receive the necessary medication. By following these 5 easy steps, you can streamline the prior authorization process and improve patient outcomes. Remember to always follow the insurance provider's specific guidelines and to keep patients informed throughout the process.

We hope this article has been informative and helpful. If you have any questions or comments, please feel free to share them below. Don't forget to share this article with your colleagues and friends who may find it useful.
What is the purpose of the Archimedes Rx Prior Authorization Form?
+The Archimedes Rx Prior Authorization Form is used to request prior authorization for prescription medications that require approval from the patient's insurance provider.
How do I submit the Archimedes Rx Prior Authorization Form?
+You can submit the form online, by fax, or by mail. Follow the insurance provider's specific submission guidelines to ensure that the form is processed quickly and efficiently.
What happens after I submit the Archimedes Rx Prior Authorization Form?
+After submitting the form, the insurance provider will review it and send a decision to the healthcare provider. The decision will indicate whether the medication is approved or denied.