Prior authorization forms can be a daunting task for many healthcare professionals and patients alike. The Arcadia prior authorization form is no exception. However, with a clear understanding of the process and the required information, filling out the form can be a relatively straightforward task. In this article, we will guide you through the 5 easy steps to fill out the Arcadia prior authorization form.
The Importance of Prior Authorization
Prior authorization is a critical step in ensuring that patients receive the necessary medical treatment while also controlling healthcare costs. It involves obtaining approval from the patient's insurance provider before administering a specific treatment or medication. The Arcadia prior authorization form is used by healthcare providers to request prior authorization for their patients.
Why is the Arcadia Prior Authorization Form Necessary?
The Arcadia prior authorization form is necessary because it helps to ensure that patients receive the most effective and efficient treatment possible. By obtaining prior authorization, healthcare providers can avoid unnecessary delays or denials of treatment. Additionally, the form helps to ensure that patients are aware of the treatment options available to them and can make informed decisions about their care.
Step 1: Gather Required Information

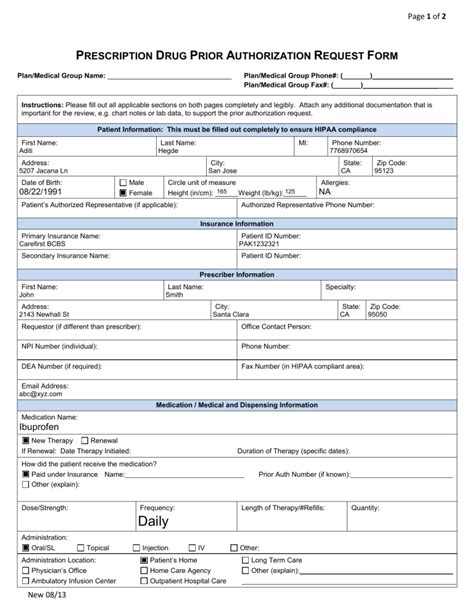
The first step in filling out the Arcadia prior authorization form is to gather all the required information. This includes:
- Patient demographics, including name, date of birth, and contact information
- Insurance information, including policy number and coverage details
- Medical history, including diagnosis and treatment information
- Treatment plan, including medication and dosages
- Supporting documentation, such as lab results or medical records
Step 2: Complete Patient Information
Completing Patient Information
The next step is to complete the patient information section of the form. This includes providing the patient's name, date of birth, and contact information. It is essential to ensure that this information is accurate and up-to-date.
- Patient name: _____________________________________________________
- Date of birth: _____________________________________________________
- Contact information: _____________________________________________________
Step 3: Complete Insurance Information
Completing Insurance Information
The insurance information section is critical in ensuring that the patient's insurance provider is notified of the prior authorization request. This section should include:
- Policy number: _____________________________________________________
- Coverage details: _____________________________________________________
- Insurance provider contact information: _____________________________________________________
Step 4: Complete Medical Information
Completing Medical Information
The medical information section is where you will provide details about the patient's medical history, diagnosis, and treatment plan. This section should include:
- Medical history: _____________________________________________________
- Diagnosis: _____________________________________________________
- Treatment plan: _____________________________________________________
- Supporting documentation: _____________________________________________________
Step 5: Review and Submit
Reviewing and Submitting the Form
The final step is to review the completed form for accuracy and completeness. Ensure that all required information is included and that the form is signed and dated. Once the form is complete, submit it to the patient's insurance provider for review and approval.

Tips and Reminders
- Ensure that all required information is included and accurate
- Use clear and concise language when completing the form
- Attach supporting documentation as necessary
- Review the form carefully before submitting it
- Follow up with the insurance provider to ensure timely approval
By following these 5 easy steps, you can ensure that the Arcadia prior authorization form is completed accurately and efficiently. Remember to gather all required information, complete the patient and insurance information sections, provide detailed medical information, review and submit the form, and follow up with the insurance provider.
We Want to Hear from You!
Have you had experience with filling out the Arcadia prior authorization form? Share your tips and insights in the comments below. Do you have any questions or concerns about the process? Let us know, and we will do our best to address them.
FAQs
What is the purpose of the Arcadia prior authorization form?
+The Arcadia prior authorization form is used to request prior authorization for medical treatment or medication.
What information is required to complete the form?
+The form requires patient demographics, insurance information, medical history, treatment plan, and supporting documentation.
How long does it take to receive approval?
+The approval time varies depending on the insurance provider and the complexity of the request.