Obtaining prior authorization for medical treatments and procedures is a crucial step in ensuring that patients receive the necessary care while minimizing out-of-pocket expenses. AmeriHealth, a leading healthcare insurance provider, requires prior authorization for certain services to ensure that patients receive medically necessary care. In this article, we will guide you through the 5-step process of completing the AmeriHealth prior authorization form.

Understanding Prior Authorization
Prior authorization is a process that healthcare providers use to obtain approval from AmeriHealth before providing certain medical services. This process ensures that patients receive medically necessary care while minimizing unnecessary expenses. Prior authorization is usually required for services such as surgeries, hospitalizations, and prescription medications.
Benefits of Prior Authorization
Prior authorization provides several benefits to patients, including:
- Ensures that patients receive medically necessary care
- Minimizes out-of-pocket expenses
- Reduces the risk of denied claims
- Streamlines the billing process
Step 1: Gather Required Information
Before starting the prior authorization process, you will need to gather some required information. This includes:
- Patient demographics (name, date of birth, etc.)
- Policy number and group number
- Diagnosis and procedure codes
- Treatment plan and duration
- Supporting medical documentation (e.g., lab results, medical records)

Important Documents to Submit
When submitting the prior authorization form, make sure to include the following documents:
- Completed prior authorization form
- Supporting medical documentation
- Treatment plan and duration
- Patient demographics and policy information
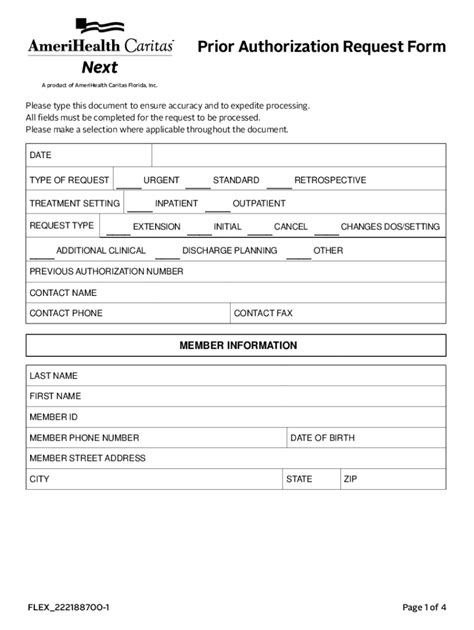
Step 2: Complete the Prior Authorization Form
The AmeriHealth prior authorization form can be obtained from the AmeriHealth website or by contacting their customer service department. The form will require you to provide the following information:
- Patient demographics
- Policy number and group number
- Diagnosis and procedure codes
- Treatment plan and duration
- Supporting medical documentation

Tips for Completing the Form
When completing the prior authorization form, make sure to:
- Use clear and concise language
- Provide accurate and complete information
- Include all required documentation
- Submit the form well in advance of the scheduled treatment date
Step 3: Submit the Prior Authorization Form
Once the prior authorization form is complete, you can submit it to AmeriHealth via fax, email, or mail. Make sure to follow the submission guidelines provided by AmeriHealth to ensure timely processing.

Submission Guidelines
When submitting the prior authorization form, make sure to:
- Use the correct fax number or email address
- Include all required documentation
- Submit the form well in advance of the scheduled treatment date
Step 4: Follow Up on the Prior Authorization Request
After submitting the prior authorization form, it's essential to follow up on the request to ensure timely processing. You can check the status of your request by contacting AmeriHealth's customer service department.

Understanding the Prior Authorization Decision
Once AmeriHealth has processed your prior authorization request, they will provide a decision. The decision may be:
- Approved: The requested service is approved, and the patient can proceed with treatment.
- Denied: The requested service is denied, and the patient may need to appeal the decision.
- Pending: The requested service is pending, and additional information is required.
Step 5: Appeal a Denied Prior Authorization Request
If your prior authorization request is denied, you may need to appeal the decision. AmeriHealth provides an appeals process for denied requests. You can appeal the decision by submitting a written appeal to AmeriHealth.

Appeals Process
When appealing a denied prior authorization request, make sure to:
- Submit a written appeal to AmeriHealth
- Include supporting medical documentation
- Explain why you disagree with the denial decision
By following these 5 steps, you can complete the AmeriHealth prior authorization form and ensure that your patients receive the necessary care while minimizing out-of-pocket expenses. Remember to gather required information, complete the form accurately, submit the form timely, follow up on the request, and appeal a denied decision if necessary.
What is prior authorization?
+Prior authorization is a process that healthcare providers use to obtain approval from AmeriHealth before providing certain medical services.
What documents are required for prior authorization?
+The required documents include the completed prior authorization form, supporting medical documentation, treatment plan and duration, and patient demographics and policy information.
How do I appeal a denied prior authorization request?
+You can appeal a denied prior authorization request by submitting a written appeal to AmeriHealth, including supporting medical documentation, and explaining why you disagree with the denial decision.