The healthcare industry has seen significant advancements in recent years, with a growing focus on providing high-quality, patient-centered care. However, navigating the complexities of healthcare can be overwhelming, especially when it comes to prior authorizations. In this article, we will delve into the world of AmeriHealth Caritas prior authorization forms, making the process easier to understand and manage.
Prior authorization, also known as pre-authorization or pre-certification, is a process used by healthcare providers and insurance companies to determine whether a particular treatment or service is medically necessary and covered under a patient's insurance plan. This process helps ensure that patients receive the most effective and efficient care while minimizing unnecessary costs.
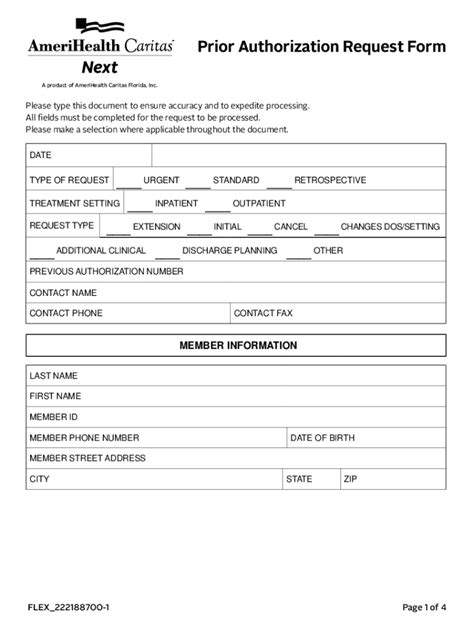
AmeriHealth Caritas, a leading health insurance provider, requires prior authorization for certain medical services and treatments. Their prior authorization form is designed to gather essential information about the patient's condition, the proposed treatment, and the medical necessity of the service. While the process may seem daunting, understanding the AmeriHealth Caritas prior authorization form can make a significant difference in ensuring that patients receive the care they need.
Understanding the AmeriHealth Caritas Prior Authorization Form

The AmeriHealth Caritas prior authorization form typically consists of several sections, each requiring specific information. The form may vary depending on the type of service or treatment being requested, but most forms will include the following:
- Patient demographics: name, date of birth, insurance ID number, and contact information
- Medical history: diagnosis, symptoms, and relevant medical conditions
- Treatment information: proposed treatment or service, including dosage and frequency
- Medical necessity: explanation of why the treatment or service is medically necessary
- Supporting documentation: relevant medical records, test results, and other supporting documents
Tips for Completing the AmeriHealth Caritas Prior Authorization Form
To ensure a smooth prior authorization process, it's essential to complete the form accurately and thoroughly. Here are some tips to help you navigate the process:
- Read the form carefully: take the time to review the form and understand what information is required
- Gather necessary documents: collect all relevant medical records, test results, and other supporting documents before starting the form
- Be detailed: provide as much information as possible about the patient's condition and the proposed treatment
- Use clear language: avoid using technical jargon or abbreviations that may be unfamiliar to the reviewer
- Submit the form promptly: ensure that the form is submitted well in advance of the proposed treatment date to avoid delays
The Benefits of Prior Authorization

While prior authorization may seem like an administrative burden, it has several benefits for patients, healthcare providers, and insurance companies. Some of the benefits include:
- Improved patient outcomes: prior authorization ensures that patients receive medically necessary treatments and services, leading to better health outcomes
- Reduced healthcare costs: prior authorization helps minimize unnecessary costs by ensuring that only medically necessary treatments are approved
- Enhanced care coordination: prior authorization facilitates communication between healthcare providers, insurance companies, and patients, leading to more coordinated care
- Increased transparency: prior authorization provides patients and healthcare providers with clear information about what is covered under the insurance plan
Common Challenges with Prior Authorization
While prior authorization is an essential process, it can be challenging to navigate. Some common challenges include:
- Delays in approval: prior authorization can cause delays in treatment, which can be frustrating for patients and healthcare providers
- Denials: prior authorization requests may be denied, which can be disappointing for patients and healthcare providers
- Administrative burden: prior authorization can be time-consuming and require significant administrative resources
AmeriHealth Caritas Prior Authorization Form Requirements

AmeriHealth Caritas has specific requirements for prior authorization forms, which may vary depending on the type of service or treatment being requested. Some common requirements include:
- Completed form: the form must be fully completed and signed by the healthcare provider
- Supporting documentation: relevant medical records, test results, and other supporting documents must be attached to the form
- Medical necessity: a clear explanation of why the treatment or service is medically necessary must be provided
- Timely submission: the form must be submitted well in advance of the proposed treatment date to avoid delays
Streamlining the Prior Authorization Process
To streamline the prior authorization process, AmeriHealth Caritas offers several resources, including:
- Online portal: healthcare providers can submit prior authorization requests online through the AmeriHealth Caritas portal
- Fax and mail: prior authorization requests can be submitted via fax or mail
- Phone support: healthcare providers can contact AmeriHealth Caritas customer support for assistance with prior authorization requests
Conclusion: Simplifying the AmeriHealth Caritas Prior Authorization Form
Prior authorization is an essential process in the healthcare industry, ensuring that patients receive medically necessary treatments and services while minimizing unnecessary costs. The AmeriHealth Caritas prior authorization form may seem daunting, but understanding the process and requirements can make a significant difference in ensuring that patients receive the care they need.
By following the tips and guidelines outlined in this article, healthcare providers can simplify the prior authorization process and reduce administrative burdens. Remember to read the form carefully, gather necessary documents, and submit the form promptly to ensure a smooth prior authorization process.
What is prior authorization, and why is it necessary?
+Prior authorization, also known as pre-authorization or pre-certification, is a process used by healthcare providers and insurance companies to determine whether a particular treatment or service is medically necessary and covered under a patient's insurance plan.
How do I complete the AmeriHealth Caritas prior authorization form?
+To complete the AmeriHealth Caritas prior authorization form, read the form carefully, gather necessary documents, and provide detailed information about the patient's condition and the proposed treatment.
What are the benefits of prior authorization?
+The benefits of prior authorization include improved patient outcomes, reduced healthcare costs, enhanced care coordination, and increased transparency.