The world of health insurance can be complex and overwhelming, especially when it comes to prior authorization. If you're a healthcare provider or patient in Florida, you may be familiar with Ambetter, a popular health insurance plan that offers affordable coverage to individuals and families. However, navigating the prior authorization process can be a challenge. In this article, we'll break down the 5 steps to Ambetter prior authorization in Florida, making it easier for you to get the care you need.
Ambetter prior authorization is a crucial step in ensuring that patients receive the necessary medical treatment while also controlling healthcare costs. By understanding the prior authorization process, healthcare providers and patients can avoid delays and ensure that medical procedures are approved in a timely manner. Whether you're a seasoned healthcare professional or a patient seeking medical attention, this article will guide you through the 5 steps to Ambetter prior authorization in Florida.
Step 1: Check the Ambetter Prior Authorization Requirements

Before starting the prior authorization process, it's essential to check the Ambetter prior authorization requirements. Healthcare providers can log in to the Ambetter provider portal to check the prior authorization requirements for specific medical procedures. Patients can also contact their healthcare provider or Ambetter customer service to determine if prior authorization is required for their medical treatment.
To check the prior authorization requirements, you'll need to have the following information:
- Patient's name and date of birth
- Medical procedure code (CPT/HCPCS)
- Diagnosis code (ICD-10)
- Ambetter policy number
Understanding the Ambetter Prior Authorization Grid
Ambetter provides a prior authorization grid that outlines the requirements for specific medical procedures. The grid is divided into three categories:
- Category 1: Procedures that require prior authorization
- Category 2: Procedures that do not require prior authorization
- Category 3: Procedures that require additional documentation
By checking the prior authorization grid, healthcare providers can determine if prior authorization is required for a specific medical procedure.
Step 2: Gather Required Documents and Information

Once you've determined that prior authorization is required, it's essential to gather the necessary documents and information. Healthcare providers will need to collect the following:
- Patient's medical history and current medical condition
- Medical procedure code (CPT/HCPCS)
- Diagnosis code (ICD-10)
- Ambetter policy number
- Treatment plan and medical records
Patients can help facilitate the process by providing their healthcare provider with the necessary documents and information.
Understanding the Importance of Accurate Information
Accurate information is crucial in the prior authorization process. Healthcare providers must ensure that all information is accurate and up-to-date to avoid delays or denials. Patients can help by providing their healthcare provider with accurate and complete information.
Step 3: Submit the Prior Authorization Request

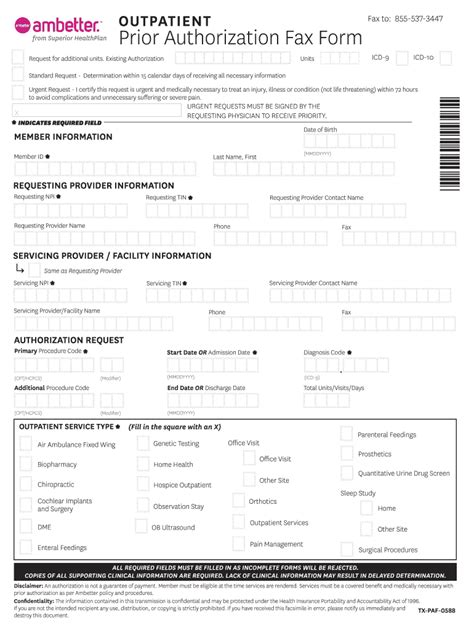
Once you've gathered the necessary documents and information, it's time to submit the prior authorization request. Healthcare providers can submit the request through the Ambetter provider portal or by fax.
To submit the request, you'll need to provide the following information:
- Patient's name and date of birth
- Medical procedure code (CPT/HCPCS)
- Diagnosis code (ICD-10)
- Ambetter policy number
- Treatment plan and medical records
Understanding the Prior Authorization Timeline
Ambetter has a specific timeline for processing prior authorization requests. Healthcare providers can expect a decision within 2-5 business days for standard requests and within 1-2 business days for expedited requests.
Step 4: Review and Respond to the Prior Authorization Decision

Once the prior authorization request has been processed, healthcare providers will receive a decision from Ambetter. If the request is approved, the healthcare provider can proceed with the medical procedure. If the request is denied, the healthcare provider can appeal the decision or provide additional information to support the request.
Patients can also appeal the decision if they disagree with the outcome.
Understanding the Appeal Process
The appeal process allows healthcare providers and patients to dispute the prior authorization decision. To appeal the decision, you'll need to provide additional information or documentation to support the request.
Step 5: Verify the Prior Authorization Status

Once the prior authorization request has been processed, it's essential to verify the status. Healthcare providers can log in to the Ambetter provider portal to check the status of the request. Patients can also contact their healthcare provider or Ambetter customer service to verify the status.
By following these 5 steps, healthcare providers and patients can navigate the Ambetter prior authorization process with ease. Remember to check the prior authorization requirements, gather required documents and information, submit the prior authorization request, review and respond to the prior authorization decision, and verify the prior authorization status.
We hope this article has been informative and helpful in guiding you through the Ambetter prior authorization process. If you have any further questions or concerns, please don't hesitate to reach out.
What is Ambetter prior authorization?
+Ambetter prior authorization is a process that requires healthcare providers to obtain approval from Ambetter before performing certain medical procedures.
How do I check the prior authorization requirements?
+Healthcare providers can log in to the Ambetter provider portal to check the prior authorization requirements for specific medical procedures.
How long does the prior authorization process take?
+Ambetter has a specific timeline for processing prior authorization requests. Healthcare providers can expect a decision within 2-5 business days for standard requests and within 1-2 business days for expedited requests.