Are you tired of dealing with the hassle of pre-authorization forms for your Ambetter health insurance? Look no further! In this article, we will guide you through the 5 easy steps to complete the Ambetter pre-authorization form, making the process smoother and less stressful for you.
Ambetter health insurance is a popular choice among individuals and families, offering a range of plans that cater to diverse needs and budgets. However, like all health insurance providers, Ambetter requires pre-authorization for certain medical procedures and treatments to ensure that they are medically necessary and covered under your plan. This is where the Ambetter pre-authorization form comes in – a crucial document that needs to be filled out and submitted to Ambetter for review.

What is the Ambetter Pre-Authorization Form?
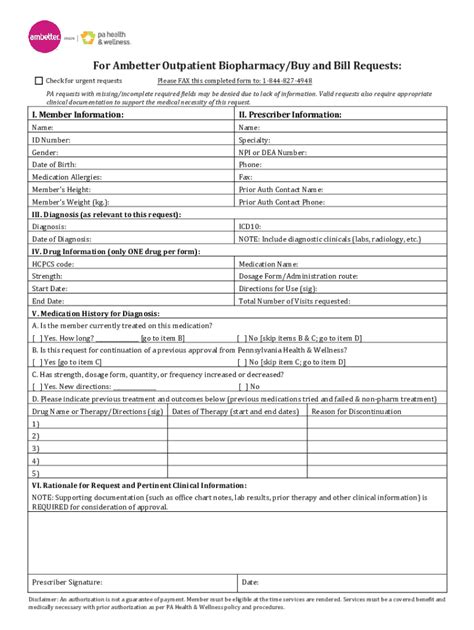
The Ambetter pre-authorization form is a document that your healthcare provider needs to fill out and submit to Ambetter before performing certain medical procedures or treatments. This form provides Ambetter with the necessary information to determine whether the proposed treatment is medically necessary and covered under your insurance plan.
Why is Pre-Authorization Required?
Pre-authorization is required to ensure that the treatment or procedure is medically necessary and aligns with Ambetter's coverage policies. This process helps to prevent unnecessary medical expenses and ensures that you receive the best possible care.
5 Easy Steps to Complete the Ambetter Pre-Authorization Form
Now that we've covered the basics, let's dive into the 5 easy steps to complete the Ambetter pre-authorization form:

Step 1: Gather Required Information
Before starting the pre-authorization process, make sure you have the following information readily available:
- Your Ambetter insurance card
- Your healthcare provider's contact information
- A detailed description of the proposed treatment or procedure
- The date and time of the scheduled treatment or procedure
Step 2: Fill Out the Pre-Authorization Form
Once you have gathered all the necessary information, fill out the Ambetter pre-authorization form. This form can be downloaded from the Ambetter website or obtained from your healthcare provider. Make sure to fill out the form accurately and completely, as incomplete or inaccurate information may delay the pre-authorization process.
Step 3: Submit the Pre-Authorization Form
After completing the pre-authorization form, submit it to Ambetter for review. You can submit the form via fax, email, or online through the Ambetter website. Make sure to keep a copy of the submitted form for your records.
Step 4: Wait for Pre-Authorization Approval
Once Ambetter receives the pre-authorization form, they will review it and determine whether the proposed treatment or procedure is medically necessary and covered under your insurance plan. This process typically takes a few days, but may take longer in some cases.
Step 5: Receive Pre-Authorization Approval or Denial
After reviewing the pre-authorization form, Ambetter will notify you and your healthcare provider of their decision. If the pre-authorization is approved, you can proceed with the scheduled treatment or procedure. If the pre-authorization is denied, you may need to appeal the decision or explore alternative treatment options.

Additional Tips and Reminders
Here are some additional tips and reminders to keep in mind when completing the Ambetter pre-authorization form:
- Make sure to submit the pre-authorization form at least 5-7 business days before the scheduled treatment or procedure.
- Keep a copy of the submitted form for your records.
- If you have any questions or concerns about the pre-authorization process, contact Ambetter customer service or your healthcare provider.
- Remember to carefully review your Ambetter insurance plan to understand what is covered and what is not.

Conclusion
Completing the Ambetter pre-authorization form is a straightforward process that requires some basic information and attention to detail. By following the 5 easy steps outlined in this article, you can ensure a smooth and hassle-free pre-authorization process. Remember to keep a copy of the submitted form for your records, and don't hesitate to reach out to Ambetter customer service or your healthcare provider if you have any questions or concerns.

We hope this article has been helpful in guiding you through the Ambetter pre-authorization form process. If you have any further questions or need additional assistance, please don't hesitate to reach out to us.
What is the purpose of the Ambetter pre-authorization form?
+The Ambetter pre-authorization form is used to determine whether a proposed medical treatment or procedure is medically necessary and covered under your insurance plan.
How long does the pre-authorization process take?
+The pre-authorization process typically takes a few days, but may take longer in some cases.
What happens if my pre-authorization is denied?
+If your pre-authorization is denied, you may need to appeal the decision or explore alternative treatment options.