Understanding the Ambetter Outpatient Prior Authorization Form: A Comprehensive Guide
For individuals enrolled in Ambetter health insurance plans, understanding the prior authorization process is crucial to ensure seamless access to medical services and treatments. The Ambetter Outpatient Prior Authorization Form is a critical document that facilitates this process, enabling healthcare providers to obtain necessary approvals before rendering certain medical services. In this article, we will delve into the intricacies of the Ambetter Outpatient Prior Authorization Form, exploring its importance, benefits, and the step-by-step process of completing and submitting it.

The Importance of Prior Authorization in Healthcare
Prior authorization is a critical component of healthcare management, ensuring that patients receive medically necessary services while controlling healthcare costs. By requiring prior authorization for certain treatments or services, health insurance providers like Ambetter can assess the necessity and effectiveness of the proposed care, preventing unnecessary expenses and optimizing resource allocation. This process also helps reduce administrative burdens on healthcare providers, allowing them to focus on delivering high-quality patient care.
Benefits of Using the Ambetter Outpatient Prior Authorization Form
The Ambetter Outpatient Prior Authorization Form offers several benefits to both healthcare providers and patients. Some of the key advantages include:
- Streamlined authorization process: The form provides a standardized format for submitting prior authorization requests, reducing administrative complexity and facilitating faster processing times.
- Improved communication: The form ensures that all relevant information is captured, promoting clear communication between healthcare providers, patients, and Ambetter representatives.
- Enhanced patient care: By ensuring that patients receive medically necessary services, the prior authorization process contributes to better health outcomes and improved patient satisfaction.
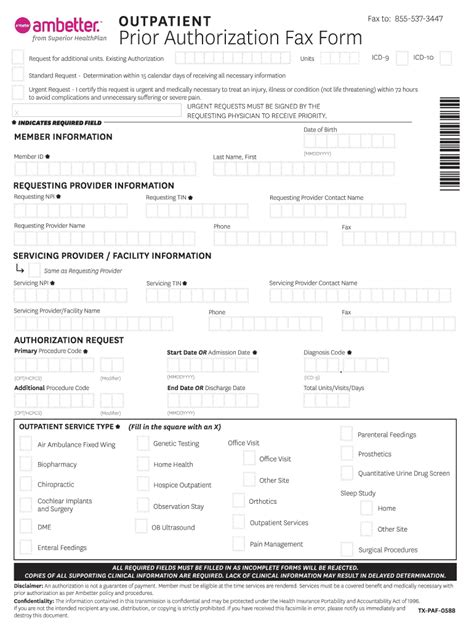
Completing and Submitting the Ambetter Outpatient Prior Authorization Form
To complete and submit the Ambetter Outpatient Prior Authorization Form, follow these steps:
- Gather required information: Ensure you have all necessary patient information, including their Ambetter ID number, medical history, and current treatment plan.
- Choose the correct form: Select the appropriate form for outpatient services, as different forms may be required for inpatient or other services.
- Fill out the form accurately: Complete the form in its entirety, providing all required information and supporting documentation.
- Attach supporting documents: Include relevant medical records, test results, or other documentation to support the prior authorization request.
- Submit the form: Fax or mail the completed form to the designated Ambetter prior authorization department.

Tips for Healthcare Providers
To ensure a smooth prior authorization process, healthcare providers should:
- Verify patient eligibility and coverage before submitting the prior authorization request.
- Ensure accurate and complete information is provided on the form.
- Submit the form well in advance of the scheduled service to allow sufficient processing time.
- Follow up with Ambetter representatives to confirm receipt and status of the prior authorization request.
Common Issues and Solutions
- Incomplete or inaccurate information: Ensure all required fields are completed accurately to avoid delays or denials.
- Insufficient supporting documentation: Provide comprehensive medical records and test results to support the prior authorization request.
- Timely submission: Submit the form in a timely manner to allow sufficient processing time before the scheduled service.

Conclusion
The Ambetter Outpatient Prior Authorization Form is a vital tool for healthcare providers and patients, ensuring that medically necessary services are delivered while controlling healthcare costs. By understanding the importance and benefits of prior authorization, healthcare providers can navigate the process with ease, completing and submitting the form accurately to facilitate seamless patient care. Remember to follow the step-by-step process, tips, and solutions outlined in this guide to ensure a smooth prior authorization experience.

Share Your Thoughts
Have you had experience with the Ambetter Outpatient Prior Authorization Form? Share your thoughts, questions, or concerns in the comments section below. Your feedback is invaluable in helping us improve this guide and provide better support to healthcare providers and patients.
FAQ Section
What is the purpose of the Ambetter Outpatient Prior Authorization Form?
+The Ambetter Outpatient Prior Authorization Form is used to obtain prior authorization for outpatient medical services, ensuring that patients receive medically necessary care while controlling healthcare costs.
How do I submit the Ambetter Outpatient Prior Authorization Form?
+The completed form can be faxed or mailed to the designated Ambetter prior authorization department.
What are the common issues and solutions when completing the Ambetter Outpatient Prior Authorization Form?
+Common issues include incomplete or inaccurate information, insufficient supporting documentation, and timely submission. Solutions include verifying patient eligibility, providing comprehensive medical records, and submitting the form in a timely manner.