The Allwell Appeal Form is an essential document for individuals who have had their Medicaid or Medicare claims denied or reduced. Understanding the appeal process can be overwhelming, but with the right guidance, you can navigate it successfully. In this article, we will provide a comprehensive, step-by-step guide on how to complete the Allwell Appeal Form.

Understanding the Allwell Appeal Form
Before we dive into the step-by-step guide, it's essential to understand the purpose of the Allwell Appeal Form. The form is used to appeal a decision made by Allwell, a Medicare Advantage plan, regarding a claim denial or reduction. The appeal process allows you to request a review of the decision and potentially have it overturned.
Why is the Allwell Appeal Form Important?
The Allwell Appeal Form is crucial because it provides a formal process for appealing a decision that may have been made in error. By completing the form, you can:
- Request a review of the decision
- Provide additional information to support your claim
- Potentially have the decision overturned
Step 1: Gather Required Information
Before starting the appeal process, it's essential to gather all the required information. This includes:
- Your Allwell policy number
- The claim number associated with the denied or reduced claim
- A detailed explanation of why you believe the decision was incorrect
- Any supporting documentation, such as medical records or bills

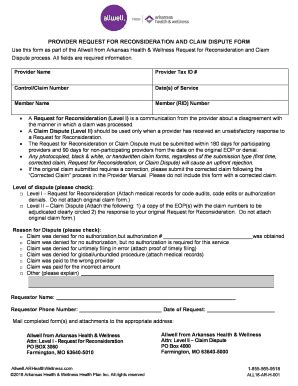
Step 2: Complete the Allwell Appeal Form
Once you have gathered all the required information, you can start completing the Allwell Appeal Form. The form typically includes the following sections:
- Section 1: Policyholder Information
- Section 2: Claim Information
- Section 3: Appeal Reason
- Section 4: Supporting Documentation
Section 1: Policyholder Information
In this section, you will need to provide your policy number, name, and contact information.
Section 2: Claim Information
In this section, you will need to provide the claim number associated with the denied or reduced claim.
Section 3: Appeal Reason
In this section, you will need to provide a detailed explanation of why you believe the decision was incorrect.
Section 4: Supporting Documentation
In this section, you will need to attach any supporting documentation, such as medical records or bills.

Step 3: Submit the Allwell Appeal Form
Once you have completed the Allwell Appeal Form, you can submit it to Allwell for review. The form can be submitted via mail, fax, or email.
Mail Submission
You can submit the form via mail to the address listed on the form.
Fax Submission
You can submit the form via fax to the number listed on the form.
Email Submission
You can submit the form via email to the email address listed on the form.

Step 4: Follow Up
After submitting the Allwell Appeal Form, it's essential to follow up with Allwell to ensure that your appeal is being processed. You can contact Allwell's customer service department to check on the status of your appeal.
What to Expect During the Appeal Process
During the appeal process, you can expect the following:
- A review of your appeal by Allwell's appeals department
- A decision regarding your appeal
- A notification of the decision via mail or email

Conclusion
The Allwell Appeal Form is an essential document for individuals who have had their Medicaid or Medicare claims denied or reduced. By following the step-by-step guide outlined in this article, you can successfully complete the form and appeal the decision.

If you have any questions or concerns about the Allwell Appeal Form or the appeal process, please don't hesitate to comment below. We are here to help.
What is the Allwell Appeal Form used for?
+The Allwell Appeal Form is used to appeal a decision made by Allwell regarding a claim denial or reduction.
How do I submit the Allwell Appeal Form?
+The form can be submitted via mail, fax, or email.
What happens after I submit the Allwell Appeal Form?
+A review of your appeal will be conducted by Allwell's appeals department, and a decision will be made regarding your appeal.