Accurate and efficient completion of insurance forms is crucial for healthcare providers and patients alike. One such form is the Aflac Form UB-04, which is used to submit claims for reimbursement. In this article, we will delve into the specifics of filling out the Aflac Form UB-04 and provide five ways to ensure accurate and efficient completion.
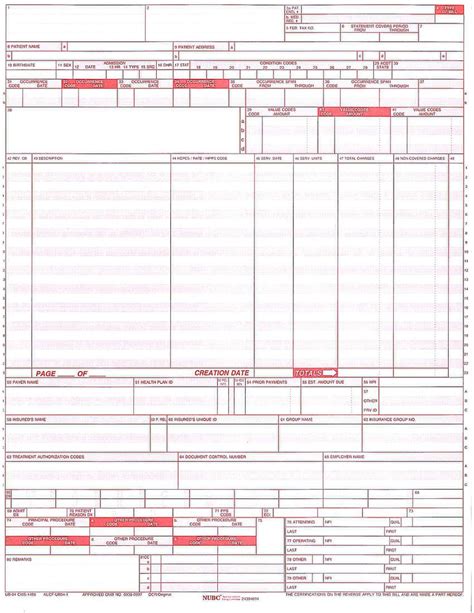
The Aflac Form UB-04, also known as the Uniform Billing Form, is a standardized form used by healthcare providers to submit claims to insurance companies, including Aflac. The form requires detailed information about the patient, the services provided, and the charges associated with those services.

Understanding the Aflac Form UB-04
Before we dive into the five ways to fill out the Aflac Form UB-04, it's essential to understand the different sections of the form. The form is divided into several sections, including:
- Patient Information
- Service Information
- Charges and Payments
- Billing Information
Each section requires specific information, and it's crucial to ensure accuracy and completeness to avoid delays or rejected claims.
1. Verify Patient Information
The first section of the Aflac Form UB-04 requires patient information, including name, address, date of birth, and policy number. It's essential to verify this information with the patient's records to ensure accuracy.

- Use the patient's identification card or records to verify the information.
- Ensure the policy number is accurate and up-to-date.
- Double-check the spelling of the patient's name and address.
Common Mistakes to Avoid
- Inaccurate or incomplete patient information can lead to delayed or rejected claims.
- Failure to verify patient information can result in incorrect billing and reimbursement.
2. Accurately Complete Service Information
The service information section requires details about the services provided, including dates, procedures, and diagnoses. It's crucial to accurately complete this section to ensure correct reimbursement.

- Use the patient's medical records to verify the services provided.
- Ensure the dates of service are accurate and complete.
- Use standardized codes, such as CPT and ICD-10, to report procedures and diagnoses.
Common Mistakes to Avoid
- Inaccurate or incomplete service information can lead to delayed or rejected claims.
- Failure to use standardized codes can result in incorrect reimbursement.
3. Calculate Charges and Payments
The charges and payments section requires the total charges for the services provided and any payments or adjustments. It's essential to accurately calculate these amounts to ensure correct reimbursement.

- Use the patient's billing records to verify the charges and payments.
- Ensure the calculations are accurate and complete.
- Apply any contractual allowances or adjustments.
Common Mistakes to Avoid
- Inaccurate or incomplete charges and payments can lead to delayed or rejected claims.
- Failure to apply contractual allowances or adjustments can result in incorrect reimbursement.
4. Complete Billing Information
The billing information section requires details about the billing provider, including name, address, and tax identification number. It's crucial to accurately complete this section to ensure correct reimbursement.

- Use the billing provider's records to verify the information.
- Ensure the tax identification number is accurate and up-to-date.
- Double-check the spelling of the billing provider's name and address.
Common Mistakes to Avoid
- Inaccurate or incomplete billing information can lead to delayed or rejected claims.
- Failure to verify billing information can result in incorrect reimbursement.
5. Review and Verify the Form
Finally, it's essential to review and verify the entire form to ensure accuracy and completeness. This includes checking for any errors or omissions and ensuring all required information is included.

- Use a checklist to ensure all required information is included.
- Double-check for any errors or omissions.
- Verify the form against the patient's records and billing information.
Common Mistakes to Avoid
- Failure to review and verify the form can lead to delayed or rejected claims.
- Inaccurate or incomplete information can result in incorrect reimbursement.
By following these five ways to fill out the Aflac Form UB-04, healthcare providers can ensure accurate and efficient completion of insurance claims. Remember to verify patient information, accurately complete service information, calculate charges and payments, complete billing information, and review and verify the form.
What is the Aflac Form UB-04?
+The Aflac Form UB-04 is a standardized form used by healthcare providers to submit claims to insurance companies, including Aflac.
What information is required on the Aflac Form UB-04?
+The form requires detailed information about the patient, the services provided, and the charges associated with those services.
How can I ensure accurate completion of the Aflac Form UB-04?
+Verify patient information, accurately complete service information, calculate charges and payments, complete billing information, and review and verify the form.
We hope this article has provided valuable insights into the Aflac Form UB-04 and how to accurately complete it. If you have any further questions or concerns, please don't hesitate to reach out.