Navigating the complexities of health insurance claims can be a daunting task for healthcare providers. One crucial aspect of this process is the Aetna reconsideration form, which allows providers to appeal denied or partially denied claims. In this article, we will delve into the world of Aetna reconsideration, exploring its importance, benefits, and a step-by-step guide on how to complete the form.

Understanding Aetna Reconsideration
Aetna reconsideration is a process that enables healthcare providers to request a review of a denied or partially denied claim. This process is essential in ensuring that patients receive the necessary care and treatment, while also protecting the rights of providers. By submitting a reconsideration form, providers can present additional information or clarify any discrepancies that may have led to the initial denial.
Benefits of Aetna Reconsideration
The Aetna reconsideration process offers several benefits to healthcare providers, including:
- The opportunity to appeal denied claims and potentially receive reimbursement
- A chance to clarify any discrepancies or provide additional information that may have been missed during the initial review
- Improved communication between providers and Aetna, leading to a better understanding of the claims process
- Enhanced patient care, as providers can continue to provide necessary treatment while the appeal is being processed
The Aetna Reconsideration Form: A Step-By-Step Guide
Completing the Aetna reconsideration form can seem like a daunting task, but by following these steps, providers can ensure a smooth and efficient process.

Step 1: Gather Necessary Information
Before starting the reconsideration form, providers should gather all necessary information, including:
- The denied or partially denied claim notification
- Patient demographics and medical records
- Billing and coding information
- Any additional documentation that supports the appeal
Step 2: Complete the Reconsideration Form
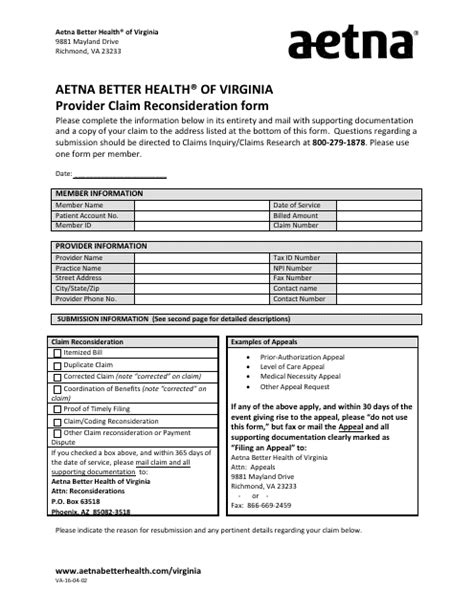
The Aetna reconsideration form typically consists of several sections, including:
- Provider information
- Patient demographics
- Claim information
- Reason for appeal
- Additional comments or documentation
Providers should carefully complete each section, ensuring that all information is accurate and up-to-date.
Step 3: Attach Supporting Documentation
Providers should attach any supporting documentation that substantiates the appeal, including:
- Medical records
- Billing and coding information
- Letters of medical necessity
- Any other relevant documentation
Step 4: Submit the Reconsideration Form
Once the reconsideration form is complete, providers should submit it to Aetna via fax, mail, or electronically. The submission method may vary depending on the provider's contract with Aetna.
Step 5: Follow Up
After submitting the reconsideration form, providers should follow up with Aetna to ensure that the appeal is being processed. This can be done via phone, email, or through Aetna's online portal.
Aetna Reconsideration Form Tips and Best Practices
To ensure a successful reconsideration process, providers should keep the following tips and best practices in mind:
- Ensure accurate and complete information on the reconsideration form
- Attach all relevant supporting documentation
- Submit the reconsideration form in a timely manner
- Follow up with Aetna to ensure the appeal is being processed
- Keep detailed records of the appeal process

Common Aetna Reconsideration Form Mistakes
Providers should be aware of common mistakes that can delay or deny the reconsideration process, including:
- Incomplete or inaccurate information on the reconsideration form
- Failure to attach supporting documentation
- Submitting the reconsideration form too late
- Not following up with Aetna
Avoiding Common Mistakes
To avoid common mistakes, providers should:
- Carefully review the reconsideration form before submission
- Ensure that all supporting documentation is attached
- Submit the reconsideration form in a timely manner
- Follow up with Aetna to ensure the appeal is being processed
Aetna Reconsideration Form FAQs
What is the Aetna reconsideration form?
+The Aetna reconsideration form is a document that allows healthcare providers to appeal denied or partially denied claims.
How do I submit the Aetna reconsideration form?
+The submission method may vary depending on the provider's contract with Aetna. Providers can submit the reconsideration form via fax, mail, or electronically.
What is the timeline for the Aetna reconsideration process?
+The timeline for the Aetna reconsideration process may vary depending on the complexity of the appeal. Providers should follow up with Aetna to ensure the appeal is being processed.
By following the steps outlined in this article and avoiding common mistakes, healthcare providers can successfully navigate the Aetna reconsideration process and ensure that their patients receive the necessary care and treatment. Remember to stay informed, stay organized, and advocate for your patients' rights. Share your experiences and tips for completing the Aetna reconsideration form in the comments below.