Aetna Medicaid Prior Authorization Form: A Comprehensive Guide
Healthcare providers play a crucial role in ensuring that patients receive the necessary medical attention and treatment. However, navigating the complexities of Medicaid prior authorization can be a daunting task, especially when dealing with large insurance providers like Aetna. In this article, we will delve into the world of Aetna Medicaid prior authorization, providing a detailed guide on the prior authorization form, its importance, and the steps involved in the process.
Understanding Aetna Medicaid Prior Authorization

Prior authorization is a process used by insurance providers to determine whether a particular treatment or service is medically necessary. In the context of Aetna Medicaid, prior authorization is required for certain medical services, procedures, and medications to ensure that patients receive the most effective and cost-efficient care.
The prior authorization process is designed to:
- Ensure that medical services are medically necessary
- Prevent unnecessary or excessive treatment
- Reduce healthcare costs
- Improve patient outcomes
The Importance of Aetna Medicaid Prior Authorization Form

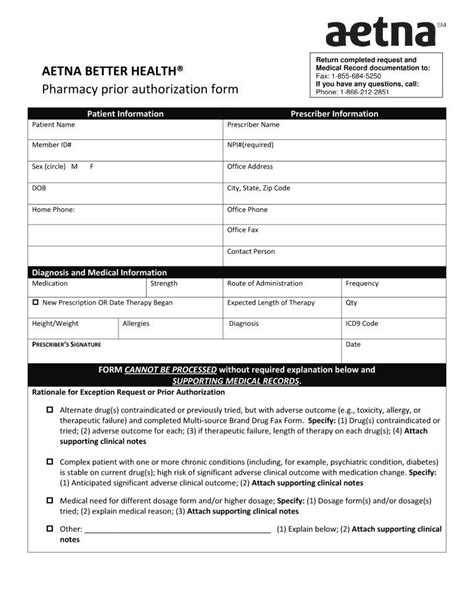
The Aetna Medicaid prior authorization form is a critical document that healthcare providers must complete and submit to Aetna for review. The form provides essential information about the patient's medical condition, treatment plan, and medical necessity. Aetna uses this information to determine whether to approve or deny the prior authorization request.
The prior authorization form typically includes:
- Patient demographics and medical history
- Treatment plan and medical necessity
- Supporting documentation, such as test results and medical records
- Healthcare provider information and credentials
Steps Involved in the Aetna Medicaid Prior Authorization Process

The Aetna Medicaid prior authorization process involves several steps:
- Determine if prior authorization is required: Healthcare providers must check Aetna's prior authorization list to determine if the medical service or treatment requires prior authorization.
- Complete the prior authorization form: Healthcare providers must complete the Aetna Medicaid prior authorization form, providing all necessary information and supporting documentation.
- Submit the prior authorization request: Healthcare providers must submit the prior authorization request to Aetna, either electronically or by mail.
- Aetna review and determination: Aetna reviews the prior authorization request and determines whether to approve or deny the request.
- Notification of determination: Aetna notifies the healthcare provider of the determination, either by phone, email, or mail.
Common Challenges and Solutions

Healthcare providers may encounter several challenges when dealing with Aetna Medicaid prior authorization. Some common challenges include:
- Delays in prior authorization processing: Aetna may take several days or weeks to process prior authorization requests, leading to delays in patient treatment.
- Denials of prior authorization requests: Aetna may deny prior authorization requests, requiring healthcare providers to resubmit the request or appeal the decision.
To overcome these challenges, healthcare providers can:
- Use electronic submission: Electronic submission of prior authorization requests can speed up the processing time.
- Ensure complete and accurate information: Providing complete and accurate information on the prior authorization form can reduce the likelihood of denials.
- Appeal denied requests: Healthcare providers can appeal denied prior authorization requests by submitting additional information or supporting documentation.
Best Practices for Aetna Medicaid Prior Authorization

To ensure a smooth prior authorization process, healthcare providers can follow these best practices:
- Stay up-to-date with Aetna's prior authorization list: Healthcare providers should regularly check Aetna's prior authorization list to ensure they are aware of any changes or updates.
- Use Aetna's online portal: Aetna's online portal can streamline the prior authorization process, reducing paperwork and increasing efficiency.
- Provide complete and accurate information: Providing complete and accurate information on the prior authorization form is essential to reduce the likelihood of denials.
Conclusion
Aetna Medicaid prior authorization is a critical process that ensures patients receive medically necessary treatment while reducing healthcare costs. By understanding the prior authorization form, the steps involved in the process, and best practices, healthcare providers can navigate the complexities of Aetna Medicaid prior authorization with ease. By following these guidelines, healthcare providers can ensure that their patients receive the necessary medical attention and treatment, while also reducing administrative burdens.
What is Aetna Medicaid prior authorization?
+Aetna Medicaid prior authorization is a process used by Aetna to determine whether a particular treatment or service is medically necessary.
What is the purpose of the Aetna Medicaid prior authorization form?
+The Aetna Medicaid prior authorization form provides essential information about the patient's medical condition, treatment plan, and medical necessity.
How do I submit a prior authorization request to Aetna?
+Prior authorization requests can be submitted electronically or by mail to Aetna.