Healthcare providers and patients often encounter complex and time-consuming processes when dealing with prior authorizations for medications. One such medication is Evenity, a treatment for osteoporosis in postmenopausal women. Aetna, a prominent health insurance provider, requires a prior authorization form for Evenity to ensure that patients meet specific criteria before receiving coverage for this medication. In this article, we will break down the Aetna Evenity prior authorization form into three easy steps, making it simpler for healthcare providers to navigate this process.
Evenity, also known as romosozumab, is a monoclonal antibody that helps to reduce the risk of fractures in postmenopausal women with osteoporosis. While this medication can be effective, it is also expensive, which is why Aetna requires prior authorization to ensure that patients meet specific clinical criteria before receiving coverage. By understanding the prior authorization process, healthcare providers can help their patients access this medication more efficiently.
Step 1: Gather Patient Information and Medical Records

The first step in completing the Aetna Evenity prior authorization form is to gather the necessary patient information and medical records. This includes:
- Patient demographics and contact information
- Medical history, including previous diagnoses and treatments
- Current medications and dosages
- Laboratory results, such as bone density scans and blood tests
- Documentation of previous osteoporosis treatments and their outcomes
Healthcare providers should ensure that they have all the necessary documents and information before proceeding with the prior authorization form. This will help to avoid delays and ensure that the form is complete and accurate.
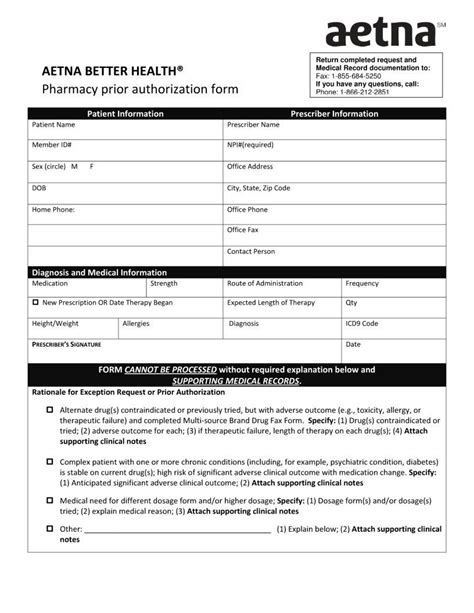
Step 2: Complete the Prior Authorization Form

The next step is to complete the Aetna Evenity prior authorization form. This form requires healthcare providers to provide detailed information about the patient's medical history, current condition, and treatment plan. The form typically includes sections on:
- Patient information and demographics
- Medical history and current condition
- Treatment plan and goals
- Laboratory results and diagnostic tests
- Previous treatments and outcomes
Healthcare providers should carefully review the form and ensure that all sections are complete and accurate. Any missing or incomplete information may result in delays or denials of prior authorization.
Step 3: Submit the Prior Authorization Form

The final step is to submit the completed prior authorization form to Aetna. Healthcare providers can submit the form via fax, mail, or online portal, depending on the preferred method. It is essential to ensure that the form is submitted correctly and that all necessary documentation is included.
Once the prior authorization form is submitted, Aetna will review the information and make a determination regarding coverage. If approved, the patient will be able to access Evenity, and the healthcare provider will receive notification of the approval. If denied, the healthcare provider may need to appeal the decision or explore alternative treatment options.
Benefits of Prior Authorization
Prior authorization may seem like a tedious process, but it has several benefits for patients and healthcare providers. Some of the benefits include:
- Improved patient outcomes: Prior authorization ensures that patients receive the most effective treatment for their condition, which can lead to better health outcomes.
- Reduced healthcare costs: By ensuring that patients meet specific clinical criteria before receiving coverage, prior authorization can help reduce healthcare costs and prevent unnecessary treatments.
- Enhanced patient safety: Prior authorization helps to prevent adverse reactions and interactions between medications, which can improve patient safety.
Tips for Healthcare Providers
To streamline the prior authorization process, healthcare providers can follow these tips:
- Stay up-to-date with prior authorization requirements: Aetna's prior authorization requirements may change over time, so it is essential to stay informed about the latest requirements.
- Use online portals for submission: Online portals can simplify the submission process and reduce errors.
- Ensure accurate and complete information: Double-check the prior authorization form for accuracy and completeness before submission.
Conclusion: Simplifying the Prior Authorization Process
The Aetna Evenity prior authorization form may seem complex, but by breaking it down into three easy steps, healthcare providers can navigate this process more efficiently. By gathering patient information and medical records, completing the prior authorization form, and submitting it correctly, healthcare providers can help their patients access this medication more quickly. Remember to stay informed about prior authorization requirements, use online portals for submission, and ensure accurate and complete information to simplify the process.
Take Action
We hope this article has helped you understand the Aetna Evenity prior authorization form and how to navigate this process. If you have any questions or comments, please share them below. Additionally, if you are a healthcare provider or patient who has experience with prior authorization, we would love to hear about your experiences and tips for simplifying this process.
FAQs
What is Evenity, and how does it work?
+Evenity, also known as romosozumab, is a monoclonal antibody that helps to reduce the risk of fractures in postmenopausal women with osteoporosis. It works by targeting a protein that breaks down bone tissue, helping to increase bone density and reduce the risk of fractures.
Why is prior authorization required for Evenity?
+Prior authorization is required for Evenity to ensure that patients meet specific clinical criteria before receiving coverage. This helps to prevent unnecessary treatments and reduces healthcare costs.
How long does the prior authorization process typically take?
+The prior authorization process typically takes several days to a week, depending on the complexity of the case and the speed of submission.