Aetna Botox Prior Authorization Form Requirements Explained

For healthcare providers and patients seeking to use Botox for various medical conditions, navigating the insurance approval process can be complex. Aetna, a leading health insurance provider, requires prior authorization for Botox treatments to ensure that patients receive medically necessary care while minimizing unnecessary costs. In this article, we will delve into the Aetna Botox prior authorization form requirements, explaining the process, necessary documents, and tips for a smooth approval.
What is Prior Authorization, and Why is it Required?
Prior authorization is a process used by health insurance providers to review the medical necessity of a treatment or medication before it is administered. This process helps ensure that patients receive only necessary and effective treatments, reducing the risk of adverse reactions, and minimizing healthcare costs. Aetna requires prior authorization for Botox treatments to verify that the treatment is medically necessary, safe, and effective for the patient's specific condition.
Aetna Botox Prior Authorization Form Requirements

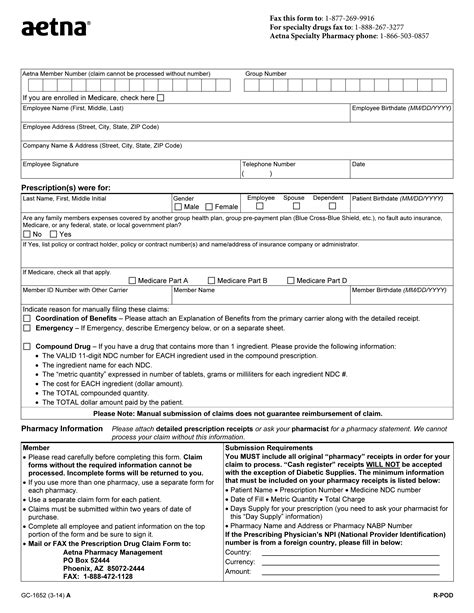
To initiate the prior authorization process, healthcare providers must submit a completed Aetna Botox prior authorization form, along with supporting documentation. The following information is typically required:
- Patient demographics and insurance information
- Diagnosis and medical condition being treated
- Botox dosage and administration details
- Treatment plan and frequency
- Medical history and relevant test results
- Supporting documentation, such as medical records, test results, and images
Documents Required for Aetna Botox Prior Authorization
To ensure a smooth prior authorization process, healthcare providers should submit the following documents:
- Completed Aetna Botox prior authorization form
- Patient's medical records, including diagnosis, medical history, and relevant test results
- Botox treatment plan, including dosage and administration details
- Supporting documentation, such as images, test results, and medical records
- Patient's insurance information and demographics
Aetna Botox Prior Authorization Process

The Aetna Botox prior authorization process typically involves the following steps:
- Submission: Healthcare providers submit the completed prior authorization form and supporting documentation to Aetna.
- Review: Aetna's clinical team reviews the submission to verify the medical necessity of the Botox treatment.
- Determination: Aetna makes a determination regarding the prior authorization request, which may be approved, denied, or require additional information.
- Notification: Aetna notifies the healthcare provider of the determination, which is typically communicated within a few days.
Tips for a Smooth Aetna Botox Prior Authorization Process
To ensure a smooth prior authorization process, healthcare providers can follow these tips:
- Submit complete and accurate information: Ensure that all required documents and information are submitted to avoid delays.
- Use the correct prior authorization form: Use the most up-to-date Aetna Botox prior authorization form to avoid rejection.
- Include supporting documentation: Submit relevant medical records, test results, and images to support the prior authorization request.
- Follow up: Contact Aetna to verify receipt of the submission and to inquire about the status of the prior authorization request.
Aetna Botox Prior Authorization FAQs

Q: What is the typical turnaround time for Aetna Botox prior authorization? A: The typical turnaround time for Aetna Botox prior authorization is 2-3 business days.
Q: Can I submit the prior authorization request electronically? A: Yes, Aetna accepts electronic submissions through their provider portal.
Q: What happens if the prior authorization request is denied? A: If the prior authorization request is denied, healthcare providers can appeal the decision by submitting additional information or supporting documentation.
Q: Can I use Botox for off-label indications? A: Aetna may consider prior authorization requests for off-label indications, but the treatment must be deemed medically necessary and supported by clinical evidence.
Conclusion
Navigating the Aetna Botox prior authorization process can be complex, but understanding the requirements and submission process can help ensure a smooth approval. By submitting complete and accurate information, including supporting documentation, healthcare providers can increase the chances of a successful prior authorization. Remember to follow up with Aetna to verify receipt of the submission and to inquire about the status of the prior authorization request.
What is the purpose of prior authorization for Botox treatments?
+The purpose of prior authorization for Botox treatments is to verify that the treatment is medically necessary, safe, and effective for the patient's specific condition.
What documents are required for Aetna Botox prior authorization?
+The required documents include a completed Aetna Botox prior authorization form, patient's medical records, Botox treatment plan, and supporting documentation such as images and test results.
How long does the Aetna Botox prior authorization process typically take?
+The typical turnaround time for Aetna Botox prior authorization is 2-3 business days.