The Wisconsin Medicaid program provides essential health coverage to low-income individuals and families, including children, pregnant women, and people with disabilities. One crucial aspect of the program is the prior authorization (PA) process, which ensures that certain medical services and medications are necessary and effective for patients. In this article, we will delve into the Wisconsin Medicaid prior authorization form guide, explaining the process, benefits, and steps involved in obtaining approval for medical treatments.
What is Prior Authorization (PA)?

Prior authorization is a process used by health insurance providers, including Wisconsin Medicaid, to determine whether a particular medical treatment or medication is medically necessary and covered under the patient's plan. The PA process involves a review of the patient's medical history, diagnosis, and treatment plan to ensure that the requested service or medication is appropriate and effective.
Benefits of Prior Authorization
The prior authorization process offers several benefits, including:
- Ensures medically necessary treatments: PA helps ensure that patients receive treatments that are medically necessary and effective for their condition.
- Reduces healthcare costs: By reviewing treatment plans and medications, PA can help reduce unnecessary healthcare expenditures.
- Promotes patient safety: PA can help prevent adverse reactions, interactions, and other safety issues related to medications and treatments.
- Enhances patient outcomes: By ensuring that patients receive evidence-based treatments, PA can improve health outcomes and quality of life.
Wisconsin Medicaid Prior Authorization Form Guide

The Wisconsin Medicaid prior authorization form guide outlines the steps and requirements for healthcare providers to obtain approval for medical treatments and medications. Here's an overview of the process:
Step 1: Determine Prior Authorization Requirements
Healthcare providers must determine whether a prior authorization is required for a specific treatment or medication. Wisconsin Medicaid has a list of services and medications that require PA, which can be found on their website.
Step 2: Gather Required Information
Providers must gather the necessary information and documentation to support the PA request, including:
- Patient demographics and medical history
- Diagnosis and treatment plan
- Medication list and dosages
- Relevant medical records and test results
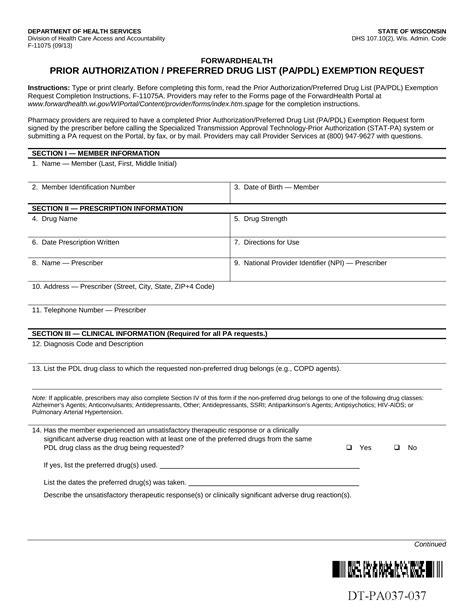
Step 3: Complete the Prior Authorization Form
Providers must complete the Wisconsin Medicaid prior authorization form, which can be found on the state's Medicaid website. The form requires detailed information about the patient, treatment plan, and medications.
Step 4: Submit the Prior Authorization Request
Providers must submit the completed PA form and supporting documentation to Wisconsin Medicaid for review. Requests can be submitted online, by phone, or by mail.
Step 5: Review and Approval
Wisconsin Medicaid will review the PA request and make a determination within a specified timeframe (usually 24-72 hours). If approved, the provider will receive a notification with the approved treatment or medication.
Common Prior Authorization Form Requirements
Here are some common requirements for the Wisconsin Medicaid prior authorization form:
- Patient's Medicaid ID number
- Provider's National Provider Identifier (NPI)
- Diagnosis code and description
- Treatment plan and medication list
- Medical records and test results
Tips for Streamlining the Prior Authorization Process

To streamline the prior authorization process, healthcare providers can follow these tips:
- Verify patient eligibility and benefits before submitting a PA request.
- Ensure accurate and complete documentation is submitted with the PA request.
- Use the Wisconsin Medicaid prior authorization form to ensure all required information is provided.
- Submit PA requests electronically to reduce processing time.
- Follow up with Wisconsin Medicaid to ensure timely review and approval.
Common Challenges and Solutions
Here are some common challenges and solutions related to the prior authorization process:
- Challenge: Delayed approvals due to incomplete or inaccurate documentation. Solution: Ensure accurate and complete documentation is submitted with the PA request.
- Challenge: Difficulty navigating the PA process. Solution: Use the Wisconsin Medicaid prior authorization form guide and online resources to streamline the process.
Wisconsin Medicaid Prior Authorization FAQs

Here are some frequently asked questions related to the Wisconsin Medicaid prior authorization process:
- Q: What services and medications require prior authorization? A: A list of services and medications that require prior authorization can be found on the Wisconsin Medicaid website.
- Q: How long does the prior authorization process take? A: The PA process typically takes 24-72 hours, but may vary depending on the complexity of the request.
- Q: Can prior authorization requests be submitted electronically? A: Yes, prior authorization requests can be submitted electronically through the Wisconsin Medicaid website.
What is the purpose of prior authorization?
+The purpose of prior authorization is to ensure that medical treatments and medications are medically necessary and effective for patients.
How do I determine if a prior authorization is required?
+Healthcare providers can determine if a prior authorization is required by checking the Wisconsin Medicaid website or contacting their Medicaid representative.
What information is required for a prior authorization request?
+Prior authorization requests require patient demographics, medical history, diagnosis, treatment plan, medication list, and relevant medical records and test results.
In conclusion, the Wisconsin Medicaid prior authorization form guide is an essential resource for healthcare providers to ensure that patients receive medically necessary and effective treatments. By understanding the PA process, benefits, and requirements, providers can streamline the process and improve patient outcomes. We encourage readers to share their experiences and tips for navigating the prior authorization process in the comments section below.