In today's healthcare landscape, obtaining prior authorization for certain medical treatments and services can be a complex and time-consuming process. Wellcare Turning Point is a program designed to provide support and resources for individuals struggling with mental health and substance use disorders. In this article, we will explore the ways to obtain Wellcare Turning Point authorization, highlighting the benefits, steps, and key information related to this process.
Why is Wellcare Turning Point Authorization Important?
Prior authorization is a critical step in ensuring that individuals receive the necessary medical treatments and services while also managing healthcare costs. Wellcare Turning Point authorization is essential for individuals struggling with mental health and substance use disorders, as it enables them to access specialized care and support services. By obtaining authorization, individuals can access a range of services, including counseling, therapy, and medication management, which are crucial for recovery and well-being.

5 Ways to Get Wellcare Turning Point Authorization
Obtaining Wellcare Turning Point authorization can be a straightforward process if you follow the right steps. Here are five ways to get authorization:
Method 1: Contact Wellcare Directly
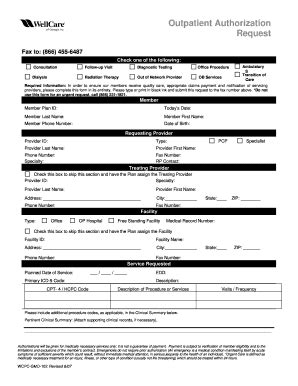
The first step in obtaining Wellcare Turning Point authorization is to contact Wellcare directly. You can reach out to their customer service department via phone or email to inquire about the authorization process. Provide them with your member ID and relevant medical information to initiate the process.
- Phone: 1-866-765-3935
- Email:
Required Documents
To initiate the authorization process, you will need to provide the following documents:
- Member ID
- Medical records
- Prescription information
- Diagnosis and treatment plan
Method 2: Use the Wellcare Website
Wellcare offers a convenient online portal where members can access their account information, check claims status, and request prior authorization. To use this method, follow these steps:
- Log in to your Wellcare account on their website
- Click on the "Prior Authorization" tab
- Fill out the online form and attach required documents
- Submit the request

Method 3: Contact Your Healthcare Provider
Your healthcare provider can also assist you in obtaining Wellcare Turning Point authorization. They can contact Wellcare on your behalf and provide the necessary medical information to support your request.
- Ask your healthcare provider to contact Wellcare's prior authorization department
- Provide your healthcare provider with your member ID and medical records
- Follow up with your healthcare provider to ensure the request is processed
Benefits of Provider-Assisted Authorization
Having your healthcare provider assist with the authorization process can have several benefits, including:
- Faster processing times
- Reduced paperwork and administrative tasks
- Increased likelihood of approval
Method 4: Use a Prior Authorization Service
Prior authorization services can help streamline the authorization process, reducing the administrative burden on healthcare providers and patients. These services can assist with:
- Eligibility verification
- Prior authorization submission
- Follow-up and appeals
Method 5: Appeal a Denied Request
If your initial request for Wellcare Turning Point authorization is denied, you can appeal the decision. To do so, follow these steps:
- Review the denial letter and understand the reason for denial
- Gather additional medical information to support your request
- Submit an appeal request to Wellcare's prior authorization department

Appeal Process Timeline
The appeal process timeline varies depending on the complexity of the case and the availability of information. On average, it can take 5-10 business days for Wellcare to review and respond to an appeal request.
Conclusion
Obtaining Wellcare Turning Point authorization can be a straightforward process if you follow the right steps. By understanding the benefits, steps, and key information related to this process, you can ensure that you receive the necessary medical treatments and services to support your recovery and well-being.
What's Next?
If you are struggling with mental health and substance use disorders, don't hesitate to reach out to Wellcare Turning Point for support. By following the steps outlined in this article, you can obtain the necessary authorization to access specialized care and support services.
Share Your Experience
Have you or a loved one struggled with mental health and substance use disorders? Share your experience and tips for obtaining Wellcare Turning Point authorization in the comments below.
FAQ Section
What is Wellcare Turning Point?
+Wellcare Turning Point is a program designed to provide support and resources for individuals struggling with mental health and substance use disorders.
How do I obtain Wellcare Turning Point authorization?
+There are five ways to obtain Wellcare Turning Point authorization: contacting Wellcare directly, using the Wellcare website, contacting your healthcare provider, using a prior authorization service, and appealing a denied request.
What documents do I need to provide for Wellcare Turning Point authorization?
+Required documents include member ID, medical records, prescription information, and diagnosis and treatment plan.