The complexities of healthcare coverage can be overwhelming, especially when it comes to navigating the system of prior authorizations. For individuals enrolled in Wellcare Medicaid, understanding the prior authorization process is crucial to ensure seamless access to necessary medical treatments and medications. In this comprehensive guide, we will delve into the world of Wellcare Medicaid prior authorization forms, explaining the importance, benefits, and step-by-step process of submitting these forms.
Understanding Wellcare Medicaid Prior Authorization
Prior authorization is a process used by health insurance providers, including Wellcare Medicaid, to determine whether a specific treatment, medication, or service is medically necessary and covered under the plan. This process aims to control healthcare costs and ensure that patients receive appropriate care. For Wellcare Medicaid beneficiaries, prior authorization is an essential step in accessing certain medical services and prescription medications.

Benefits of Prior Authorization
While the prior authorization process may seem like an additional hurdle, it offers several benefits to patients and healthcare providers alike. Some of the key advantages include:
- Cost savings: By reviewing the medical necessity of treatments and medications, prior authorization helps reduce unnecessary healthcare spending.
- Improved patient outcomes: Prior authorization ensures that patients receive evidence-based treatments that are likely to be effective for their specific condition.
- Reduced risk of adverse interactions: By reviewing medication requests, prior authorization helps minimize the risk of adverse interactions between different medications.
The Prior Authorization Process for Wellcare Medicaid
The prior authorization process for Wellcare Medicaid involves several steps, which are outlined below:
Step 1: Determine If Prior Authorization Is Required
Not all medical services or medications require prior authorization. Wellcare Medicaid beneficiaries and their healthcare providers can check the Wellcare website or contact the company's customer service department to determine if prior authorization is necessary.

Step 2: Gather Required Information
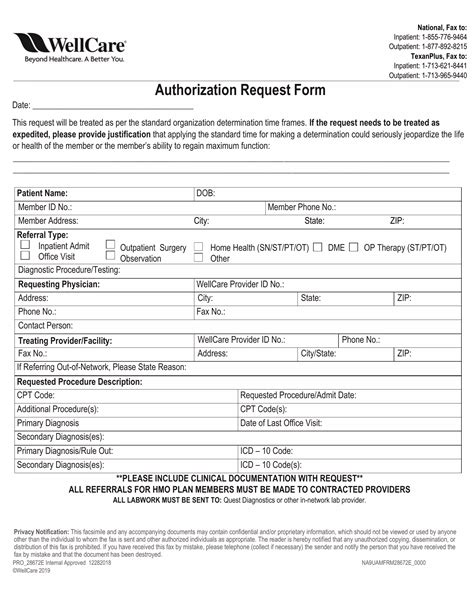
To initiate the prior authorization process, healthcare providers will need to gather relevant information about the patient's condition, treatment history, and the requested service or medication. This may include:
- Patient demographics and contact information
- Medical history and current condition
- Treatment plan and requested service or medication
- Supporting documentation, such as medical records or test results
Step 3: Submit the Prior Authorization Request
Once the necessary information is gathered, the healthcare provider can submit the prior authorization request to Wellcare Medicaid. This can typically be done online, by phone, or by mail.

Step 4: Review and Determination
Wellcare Medicaid will review the prior authorization request to determine whether the requested service or medication is medically necessary and covered under the plan. This review process typically takes a few days to a week.
Step 5: Notification of Determination
Once the prior authorization request has been reviewed, Wellcare Medicaid will notify the healthcare provider and patient of the determination. If the request is approved, the patient can proceed with the treatment or medication. If the request is denied, the patient and healthcare provider can appeal the decision.

Tips for Submitting a Successful Prior Authorization Request
To increase the chances of a successful prior authorization request, healthcare providers and patients can follow these tips:
- Ensure complete and accurate information: Make sure all required information is gathered and submitted with the prior authorization request.
- Provide supporting documentation: Include relevant medical records, test results, and other supporting documentation to help justify the requested service or medication.
- Follow up: If the prior authorization request is delayed or denied, follow up with Wellcare Medicaid to resolve any issues.

Conclusion
Navigating the prior authorization process for Wellcare Medicaid can seem daunting, but by understanding the benefits, steps, and requirements, patients and healthcare providers can work together to ensure seamless access to necessary medical treatments and medications. By following the tips outlined in this guide, individuals can increase their chances of a successful prior authorization request.
We hope this comprehensive guide has provided valuable insights into the world of Wellcare Medicaid prior authorization forms. If you have any further questions or concerns, please don't hesitate to reach out.
Share your thoughts and experiences with prior authorization in the comments below!
What is prior authorization, and why is it necessary?
+Prior authorization is a process used by health insurance providers to determine whether a specific treatment, medication, or service is medically necessary and covered under the plan. It helps control healthcare costs and ensures that patients receive appropriate care.
How do I determine if prior authorization is required for a specific service or medication?
+You can check the Wellcare website or contact the company's customer service department to determine if prior authorization is necessary for a specific service or medication.
What information do I need to gather for a prior authorization request?
+You will need to gather relevant information about the patient's condition, treatment history, and the requested service or medication. This may include patient demographics, medical history, treatment plan, and supporting documentation.