Navigating the complexities of healthcare and insurance can be overwhelming, especially when dealing with denied claims or disputed coverage. Allwell, a well-established Medicare Advantage plan provider, offers its members a comprehensive appeal process to ensure that their concerns are heard and addressed. Understanding the Allwell Wellcare appeal form and process is crucial for members who wish to dispute a coverage decision or a denied claim. In this article, we will delve into the details of the Allwell Wellcare appeal form, providing a step-by-step guide to help you navigate this process efficiently.

Why Is the Appeal Process Important?
The appeal process is a critical component of healthcare insurance, as it allows members to dispute decisions made by their insurance provider. This process is designed to ensure that members receive fair and adequate coverage for the medical services they require. By understanding and utilizing the appeal process, members can advocate for themselves and ensure that their healthcare needs are met.
Understanding the Allwell Wellcare Appeal Form
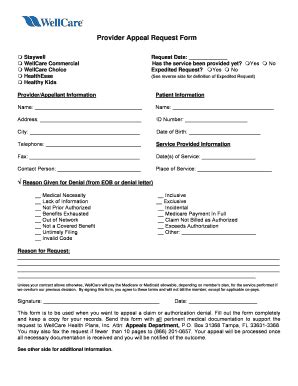
The Allwell Wellcare appeal form is a document that members must complete and submit when disputing a coverage decision or a denied claim. This form provides Allwell with the necessary information to review and address the member's concerns. The appeal form typically requires members to provide detailed information about their dispute, including the reason for the appeal, the date of the disputed decision, and any supporting documentation.

Step-by-Step Guide to Completing the Allwell Wellcare Appeal Form
Completing the Allwell Wellcare appeal form requires careful attention to detail and a thorough understanding of the appeal process. Here is a step-by-step guide to help you navigate this process:
Step 1: Review the Disputed Decision
Before starting the appeal process, carefully review the disputed decision or denied claim. Ensure that you understand the reason for the denial and the specific services or treatments that were denied.
Step 2: Gather Supporting Documentation
Collect any supporting documentation that may be relevant to your appeal, such as medical records, test results, or correspondence with your healthcare provider. This documentation will help to strengthen your case and provide context for your dispute.
Step 3: Complete the Appeal Form
Obtain a copy of the Allwell Wellcare appeal form, either by downloading it from the Allwell website or by requesting a copy from Allwell's customer service department. Carefully complete the form, ensuring that you provide all required information and documentation.
Step 4: Submit the Appeal Form
Submit the completed appeal form to Allwell, either by mail or fax, depending on the specified instructions. Ensure that you retain a copy of the form and any supporting documentation for your records.
Step 5: Wait for a Decision
After submitting the appeal form, wait for a decision from Allwell. This process typically takes several weeks, but may vary depending on the complexity of the dispute.
Types of Appeals
There are several types of appeals that members may file, including:
- Pre-Service Appeals: These appeals are filed before receiving medical services, typically to dispute a denial of coverage for a specific treatment or service.
- Post-Service Appeals: These appeals are filed after receiving medical services, typically to dispute a denied claim or a disputed bill.
- Reconsideration Appeals: These appeals are filed when a member disagrees with a decision made by Allwell, typically after a previous appeal has been denied.
Additional Tips and Considerations
- Seek Support: Consider seeking support from a healthcare advocate or a patient representative, who can help guide you through the appeal process.
- Stay Organized: Keep detailed records of your appeal, including dates, times, and correspondence with Allwell.
- Follow Up: Follow up with Allwell to ensure that your appeal is being processed and to inquire about the status of your case.

Conclusion: Taking Control of Your Healthcare
Navigating the Allwell Wellcare appeal process may seem daunting, but by understanding the appeal form and following these steps, you can take control of your healthcare and ensure that your concerns are heard. Remember to stay organized, seek support when needed, and follow up with Allwell to ensure that your appeal is being processed efficiently.

We Encourage You to Share Your Thoughts
Have you had experience with the Allwell Wellcare appeal process? Share your thoughts and insights in the comments below. Your feedback can help others navigate this complex process and advocate for themselves.
What is the purpose of the Allwell Wellcare appeal form?
+The Allwell Wellcare appeal form is used to dispute a coverage decision or a denied claim. It provides Allwell with the necessary information to review and address the member's concerns.
How long does the appeal process typically take?
+The appeal process typically takes several weeks, but may vary depending on the complexity of the dispute.
Can I seek support during the appeal process?
+Yes, consider seeking support from a healthcare advocate or a patient representative, who can help guide you through the appeal process.