The Virginia Medicaid program provides essential health coverage to low-income individuals and families across the state. To ensure that beneficiaries receive necessary medical care while controlling costs, the program requires prior authorization for certain medications, treatments, and services. In this comprehensive guide, we will walk you through the Virginia Medicaid prior authorization form process, highlighting its importance, benefits, and step-by-step instructions for healthcare providers and patients.
Importance of Prior Authorization in Virginia Medicaid
Prior authorization is a critical component of the Virginia Medicaid program, as it helps to:
- Ensure that beneficiaries receive medically necessary care
- Prevent unnecessary or excessive utilization of services
- Control program costs and allocate resources efficiently
- Promote effective communication between healthcare providers, patients, and the Medicaid program
Benefits of Prior Authorization for Healthcare Providers and Patients
Prior authorization offers several benefits for both healthcare providers and patients, including:
- Improved patient outcomes through timely access to necessary care
- Enhanced care coordination and collaboration between healthcare providers
- Reduced administrative burden and costs for healthcare providers
- Increased transparency and accountability in the Medicaid program

Prior Authorization Process for Healthcare Providers
To obtain prior authorization for a Virginia Medicaid beneficiary, healthcare providers must follow these steps:
- Determine if prior authorization is required: Check the Virginia Medicaid website or consult with the program's customer service to determine if prior authorization is required for a specific medication, treatment, or service.
- Gather necessary documentation: Collect all relevant medical records, test results, and other documentation to support the prior authorization request.
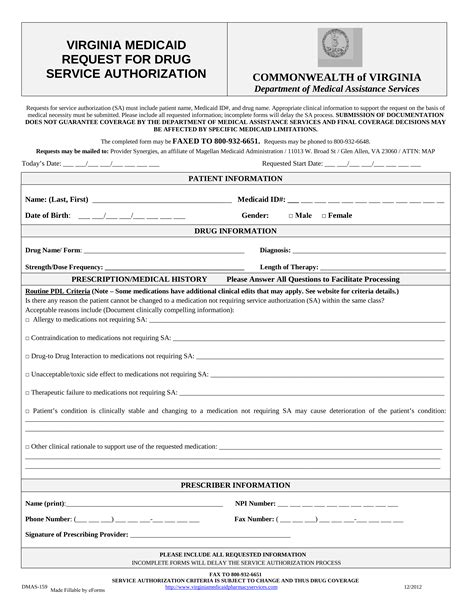
- Complete the prior authorization form: Download and complete the Virginia Medicaid prior authorization form, which can be found on the program's website.
- Submit the request: Fax or electronically submit the prior authorization request to the Virginia Medicaid program.
Virginia Medicaid Prior Authorization Form Requirements
The prior authorization form requires healthcare providers to provide detailed information about the beneficiary, the requested service or medication, and the medical justification for the request. The form typically includes the following sections:
- Beneficiary information: Name, date of birth, Medicaid ID number, and contact information
- Service or medication information: Description of the requested service or medication, including dosage and frequency
- Medical justification: Clinical rationale for the requested service or medication, including relevant medical history and test results
- Supporting documentation: Attachments of relevant medical records, test results, and other documentation
Tips for Successful Prior Authorization Requests
To increase the likelihood of a successful prior authorization request, healthcare providers should:
- Ensure accuracy and completeness: Verify that all required information is accurate and complete
- Provide clear medical justification: Clearly explain the medical rationale for the requested service or medication
- Attach relevant documentation: Include all relevant medical records, test results, and other documentation to support the request

Prior Authorization Timeline and Decision Process
The Virginia Medicaid program typically processes prior authorization requests within 24-48 hours. However, this timeframe may vary depending on the complexity of the request and the availability of necessary documentation. If additional information is required, the program will notify the healthcare provider and request the necessary documentation.
Once the prior authorization request is processed, the program will make a determination based on medical necessity and program guidelines. If the request is approved, the healthcare provider will receive notification, and the beneficiary will be able to receive the authorized service or medication. If the request is denied, the healthcare provider will receive notification, and the beneficiary may appeal the decision.

Common Prior Authorization Denial Reasons
Prior authorization requests may be denied for various reasons, including:
- Lack of medical necessity: The requested service or medication is not medically necessary
- Insufficient documentation: The request lacks necessary documentation or information
- Non-compliance with program guidelines: The requested service or medication does not comply with program guidelines or policies
Appealing a Prior Authorization Denial
If a prior authorization request is denied, beneficiaries or healthcare providers may appeal the decision by submitting a written appeal to the Virginia Medicaid program. The appeal should include:
- Reasons for appeal: Clearly explain the reasons for appealing the denial
- Additional documentation: Provide any additional documentation or information that supports the appeal

Conclusion
The Virginia Medicaid prior authorization form process is an essential component of the program, ensuring that beneficiaries receive medically necessary care while controlling costs. By understanding the prior authorization process, benefits, and requirements, healthcare providers can successfully navigate the system and provide high-quality care to their patients. If you have any questions or concerns about the prior authorization process, we encourage you to comment below or share this article with your colleagues and patients.
What is the purpose of prior authorization in the Virginia Medicaid program?
+Prior authorization is a critical component of the Virginia Medicaid program, ensuring that beneficiaries receive medically necessary care while controlling costs and promoting effective communication between healthcare providers, patients, and the Medicaid program.
How do I determine if prior authorization is required for a specific medication or treatment?
+Check the Virginia Medicaid website or consult with the program's customer service to determine if prior authorization is required for a specific medication or treatment.
What information is required on the prior authorization form?
+The prior authorization form requires healthcare providers to provide detailed information about the beneficiary, the requested service or medication, and the medical justification for the request.