Prior authorization forms are a crucial part of the healthcare system, allowing healthcare providers to request approval from insurance companies before administering specific treatments or services. One such form is the Turning Point prior authorization form, which is used by healthcare providers to request approval for patients receiving care at Turning Point facilities. In this article, we will delve into the requirements for the Turning Point prior authorization form, exploring its importance, benefits, and the step-by-step process of completion.
The Importance of Prior Authorization Forms
Prior authorization forms are essential in the healthcare industry as they ensure that patients receive necessary treatments while also controlling healthcare costs. These forms allow insurance companies to review the medical necessity of a treatment or service, ensuring that it is aligned with their coverage policies. By requiring prior authorization, insurance companies can prevent unnecessary treatments, reduce costs, and improve patient outcomes.
Benefits of Prior Authorization Forms
Prior authorization forms offer several benefits to healthcare providers, insurance companies, and patients. Some of these benefits include:
- Reduced costs: By reviewing treatment plans before they are administered, insurance companies can prevent unnecessary costs.
- Improved patient outcomes: Prior authorization forms ensure that patients receive medically necessary treatments, leading to better health outcomes.
- Enhanced communication: Prior authorization forms facilitate communication between healthcare providers and insurance companies, ensuring that all parties are informed about treatment plans.
Turning Point Prior Authorization Form Requirements
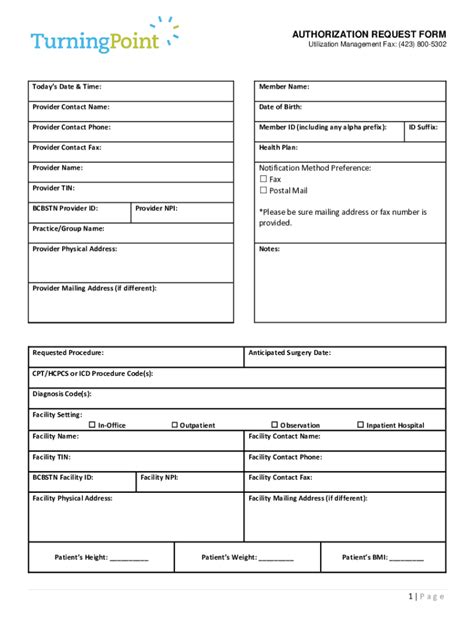
The Turning Point prior authorization form is used by healthcare providers to request approval for patients receiving care at Turning Point facilities. The form requires specific information to ensure that the request is processed efficiently. Some of the key requirements include:
- Patient demographics: The form requires patient demographics, including name, date of birth, and contact information.
- Treatment information: The form requires detailed information about the treatment or service being requested, including the type of treatment, duration, and frequency.
- Medical necessity: The form requires documentation of the medical necessity of the treatment or service, including diagnoses, test results, and treatment plans.

Step-by-Step Process of Completion
Completing the Turning Point prior authorization form requires careful attention to detail. Here is a step-by-step guide to help healthcare providers complete the form:
- Gather required information: Before starting the form, gather all required information, including patient demographics, treatment information, and medical necessity documentation.
- Complete patient demographics: Fill in the patient demographics section, including name, date of birth, and contact information.
- Provide treatment information: Fill in the treatment information section, including the type of treatment, duration, and frequency.
- Document medical necessity: Attach documentation of the medical necessity of the treatment or service, including diagnoses, test results, and treatment plans.
- Submit the form: Submit the completed form to the insurance company for review and approval.

Tips for Efficient Completion
Completing the Turning Point prior authorization form efficiently requires careful planning and attention to detail. Here are some tips to help healthcare providers complete the form efficiently:
- Use a template: Use a template to ensure that all required information is included.
- Attach supporting documentation: Attach supporting documentation, including diagnoses, test results, and treatment plans.
- Submit the form electronically: Submit the form electronically to reduce processing time.

Common Mistakes to Avoid
Completing the Turning Point prior authorization form requires careful attention to detail. Here are some common mistakes to avoid:
- Incomplete information: Ensure that all required information is included, including patient demographics, treatment information, and medical necessity documentation.
- Inaccurate information: Ensure that all information is accurate, including patient demographics, treatment information, and medical necessity documentation.

Best Practices for Turning Point Prior Authorization Form
Here are some best practices for completing the Turning Point prior authorization form:
- Use clear and concise language: Use clear and concise language when completing the form.
- Attach supporting documentation: Attach supporting documentation, including diagnoses, test results, and treatment plans.

Conclusion and Final Thoughts
The Turning Point prior authorization form is a crucial part of the healthcare system, allowing healthcare providers to request approval from insurance companies before administering specific treatments or services. By following the step-by-step process of completion and avoiding common mistakes, healthcare providers can ensure that the form is completed efficiently and accurately. By using best practices and attaching supporting documentation, healthcare providers can ensure that patients receive necessary treatments while also controlling healthcare costs.
We hope this article has provided valuable insights into the Turning Point prior authorization form requirements. If you have any questions or comments, please feel free to share them below.
What is the purpose of the Turning Point prior authorization form?
+The Turning Point prior authorization form is used by healthcare providers to request approval from insurance companies before administering specific treatments or services.
What information is required on the Turning Point prior authorization form?
+The form requires patient demographics, treatment information, and medical necessity documentation.
How can healthcare providers complete the Turning Point prior authorization form efficiently?
+Healthcare providers can complete the form efficiently by using a template, attaching supporting documentation, and submitting the form electronically.