Navigating the complexities of health insurance claims can be a daunting task, especially when dealing with unexpected medical bills. The Tufts Claim Review Form is an essential tool for individuals seeking reimbursement for medical expenses. In this article, we will delve into the intricacies of the Tufts Claim Review Form, providing a step-by-step guide to help you navigate the process with ease.
Understanding the Tufts Claim Review Form

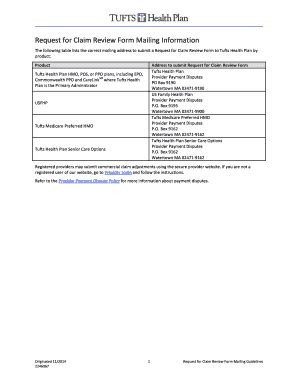
The Tufts Claim Review Form is a document used by Tufts Health Plan, a non-profit health insurance organization, to review and process medical claims. The form is designed to provide a clear and concise way for members to submit claims for reimbursement. By understanding the purpose and structure of the form, you can ensure a smooth and efficient claims process.
Benefits of Using the Tufts Claim Review Form
- Streamlined claims process: The form provides a clear and concise way to submit claims, reducing the risk of errors and delays.
- Easy to use: The form is designed to be user-friendly, making it easy for members to navigate and complete.
- Faster reimbursement: By providing all necessary information upfront, you can expedite the reimbursement process.
Step-by-Step Guide to Completing the Tufts Claim Review Form

To ensure a smooth claims process, follow these steps to complete the Tufts Claim Review Form:
- Gather necessary documents: Before starting the form, make sure you have all necessary documents, including:
- Medical bills and receipts
- Insurance cards and identification
- Proof of payment (if applicable)
- Fill out Section 1: Member Information: Provide your name, address, and Tufts Health Plan member ID number.
- Fill out Section 2: Claim Information: Provide details about the medical service or treatment, including:
- Date of service
- Provider name and address
- Type of service (e.g., doctor visit, hospital stay)
- Fill out Section 3: Payment Information: Provide details about any payments made, including:
- Amount paid
- Date paid
- Payment method (e.g., check, credit card)
- Attach supporting documentation: Attach all necessary documents, including medical bills and receipts.
- Review and sign the form: Carefully review the form for accuracy and completeness. Sign and date the form.
Tips for Completing the Tufts Claim Review Form
- Make sure to complete all sections of the form.
- Use black ink to sign the form.
- Attach all necessary documentation to avoid delays.
- Keep a copy of the completed form for your records.
Common Mistakes to Avoid When Completing the Tufts Claim Review Form

To avoid delays or rejection of your claim, avoid the following common mistakes:
- Incomplete or inaccurate information
- Missing or unsigned documentation
- Failure to attach supporting documentation
- Using pencil or pen other than black ink to sign the form
What to Expect After Submitting the Tufts Claim Review Form
- Processing time: Allow 2-4 weeks for Tufts Health Plan to process your claim.
- Reimbursement: If your claim is approved, you can expect reimbursement within 2-4 weeks.
- Denial or partial denial: If your claim is denied or partially denied, you will receive a letter explaining the reason for the denial.
Conclusion

The Tufts Claim Review Form is a valuable tool for individuals seeking reimbursement for medical expenses. By following the step-by-step guide and avoiding common mistakes, you can ensure a smooth and efficient claims process. If you have any questions or concerns, don't hesitate to reach out to Tufts Health Plan for assistance.
We encourage you to share your experiences with the Tufts Claim Review Form in the comments below. Have you had any issues or success with the form? Share your story to help others navigate the process.
What is the Tufts Claim Review Form used for?
+The Tufts Claim Review Form is used to review and process medical claims for reimbursement.
How long does it take to process a claim?
+Allow 2-4 weeks for Tufts Health Plan to process your claim.
What happens if my claim is denied?
+If your claim is denied, you will receive a letter explaining the reason for the denial.