Streamlining Tricare Prior Authorization Referral Form: A Simplified Guide

Navigating the complexities of healthcare can be overwhelming, especially when it comes to dealing with insurance providers. Tricare, the healthcare program for uniformed service members, retirees, and their families, has its own set of procedures to ensure that beneficiaries receive the necessary medical care. One crucial aspect of this process is the prior authorization referral form, which can often be a source of confusion. In this article, we will break down the Tricare prior authorization referral form, making it easier to understand and complete.
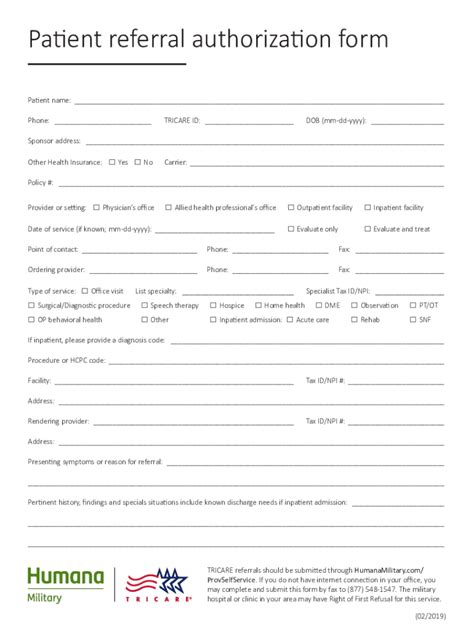
Tricare prior authorization is a requirement for certain medical services, including specialist care, surgeries, and some prescriptions. This process ensures that the treatment is medically necessary and meets Tricare's coverage guidelines. The prior authorization referral form is a critical document that facilitates communication between healthcare providers, patients, and Tricare. However, the form's complexity can lead to frustration and delays in care. By understanding the form's components and the submission process, beneficiaries can navigate this system more efficiently.
Understanding the Tricare Prior Authorization Referral Form

The Tricare prior authorization referral form typically includes the following sections:
- Patient information: Name, date of birth, and Tricare ID number
- Provider information: Name, address, and contact details
- Referring provider information: Name, address, and contact details
- Procedure or service information: Description of the requested service, including codes and diagnoses
- Clinical information: Relevant medical history, test results, and treatment plans
Benefits of Electronic Prior Authorization

In recent years, Tricare has transitioned to electronic prior authorization, which offers several benefits:
- Faster processing times: Electronic submissions reduce the time it takes to review and approve requests
- Reduced errors: Automated systems minimize the risk of errors and lost paperwork
- Increased efficiency: Providers can track the status of requests and receive notifications in real-time
To take advantage of electronic prior authorization, providers can use Tricare's online portal or third-party software solutions. These systems guide users through the submission process, ensuring that all required information is included.
Step-by-Step Guide to Completing the Tricare Prior Authorization Referral Form

To complete the Tricare prior authorization referral form, follow these steps:
- Gather required information: Collect patient, provider, and procedure details
- Choose the correct form: Ensure you are using the most up-to-date version of the form
- Fill out the form accurately: Double-check all information for errors
- Attach supporting documentation: Include relevant medical records and test results
- Submit the form: Use Tricare's online portal or third-party software solutions for electronic submission
Common Mistakes to Avoid When Completing the Tricare Prior Authorization Referral Form

When completing the Tricare prior authorization referral form, be aware of the following common mistakes:
- Incomplete or inaccurate information
- Missing or incorrect provider codes
- Insufficient clinical information
- Delayed or incomplete submission
To avoid these mistakes, carefully review the form before submission and ensure that all required information is included.
Tricare Prior Authorization Referral Form FAQs

Q: What is the purpose of the Tricare prior authorization referral form? A: The form is used to request approval for certain medical services, ensuring that they meet Tricare's coverage guidelines.
Q: How long does it take to process a prior authorization request? A: Processing times vary, but electronic submissions are typically faster than paper submissions.
Q: Can I submit the form online? A: Yes, Tricare offers an online portal for electronic submissions.
Q: What happens if my request is denied? A: You can appeal the decision by submitting additional information or clarification.
By understanding the Tricare prior authorization referral form and following the steps outlined in this article, beneficiaries can navigate the process more efficiently. Remember to avoid common mistakes and take advantage of electronic prior authorization to streamline the submission process.
Next Steps: Take Control of Your Tricare Prior Authorization Referral Form

Now that you have a better understanding of the Tricare prior authorization referral form, take control of your healthcare by:
- Familiarizing yourself with Tricare's policies and procedures
- Working closely with your healthcare provider to ensure accurate and complete submissions
- Utilizing electronic prior authorization to reduce processing times and errors
- Appealing any denied requests to ensure you receive the necessary medical care
By being proactive and informed, you can ensure a smoother experience when dealing with Tricare's prior authorization process.
We invite you to share your experiences and tips for navigating the Tricare prior authorization referral form process in the comments section below. Your insights can help others who may be facing similar challenges.