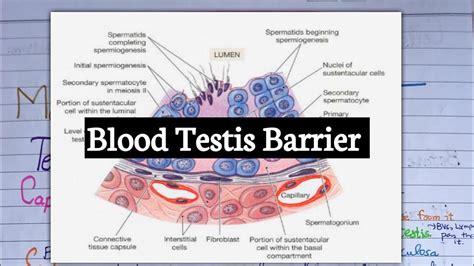
The blood-testis barrier (BTB) is a crucial structure in the testes that separates the seminiferous tubules from the bloodstream, playing a vital role in spermatogenesis and immune protection. Among the various cell types that contribute to the formation of the BTB, sustentacular cells, also known as Sertoli cells, are the most prominent. These cells are responsible for creating and maintaining the BTB, ensuring the health and integrity of the seminiferous tubules.
The blood-testis barrier is a complex structure composed of multiple layers, including the basement membrane, the tight junctions between Sertoli cells, and the actin-based cytoskeleton. The BTB serves as a physical and immunological barrier, preventing the passage of toxins, pathogens, and immune cells into the seminiferous tubules, where sperm are produced. This barrier also regulates the transport of nutrients, hormones, and other essential molecules necessary for spermatogenesis.

Sustentacular cells are somatic cells that surround the developing sperm cells, providing them with essential nutrients, growth factors, and structural support. These cells are connected by tight junctions, which form the primary component of the BTB. The tight junctions between Sertoli cells are dynamic structures that can open and close to regulate the passage of molecules across the BTB.
Functions of Sustentacular Cells in the Blood-Testis Barrier
Sustentacular cells play multiple roles in the maintenance of the BTB and the regulation of spermatogenesis. Some of the key functions of these cells include:

- Nutrient and hormone transport: Sustentacular cells regulate the transport of essential nutrients, hormones, and growth factors to the developing sperm cells.
- Immune protection: The BTB formed by sustentacular cells prevents the entry of immune cells and pathogens into the seminiferous tubules, protecting the developing sperm from immune attack.
- Structural support: Sustentacular cells provide structural support to the developing sperm cells, maintaining their shape and integrity.
- Tight junction formation: Sustentacular cells form tight junctions with neighboring cells, creating a physical barrier that regulates the passage of molecules across the BTB.
Mechanisms of Tight Junction Formation
The formation of tight junctions between sustentacular cells is a complex process involving multiple proteins and signaling pathways. Some of the key mechanisms involved in tight junction formation include:
- Cadherin-based adhesion: Cadherins are a family of adhesion molecules that play a crucial role in the formation of tight junctions between Sertoli cells.
- Catenin-based signaling: Catenins are a family of proteins that interact with cadherins to regulate tight junction formation and maintenance.
- Rho GTPase signaling: Rho GTPases are a family of proteins that regulate actin cytoskeleton dynamics and tight junction formation.

Regulation of the Blood-Testis Barrier
The BTB is a dynamic structure that is regulated by multiple hormones and signaling pathways. Some of the key regulators of the BTB include:
- Androgens: Androgens, such as testosterone, play a crucial role in regulating the BTB and spermatogenesis.
- Estrogens: Estrogens, such as estradiol, also regulate the BTB and spermatogenesis.
- Cytokines: Cytokines, such as interleukin-1 and tumor necrosis factor-alpha, can disrupt the BTB and impair spermatogenesis.

Implications for Reproductive Health
Dysfunction of the BTB has been implicated in various reproductive disorders, including infertility, testicular cancer, and autoimmune orchitis. Understanding the mechanisms of BTB formation and regulation is essential for developing novel therapeutic strategies to treat these disorders.
Therapeutic Strategies
Some potential therapeutic strategies for treating BTB-related disorders include:
- Hormone therapy: Hormone replacement therapy may be effective in regulating the BTB and improving spermatogenesis.
- Immunotherapy: Immunotherapy may be effective in treating autoimmune disorders that disrupt the BTB.
- Stem cell therapy: Stem cell therapy may be effective in repairing damaged Sertoli cells and restoring the BTB.

In conclusion, sustentacular cells play a crucial role in forming and maintaining the blood-testis barrier, regulating spermatogenesis and immune protection. Understanding the mechanisms of BTB formation and regulation is essential for developing novel therapeutic strategies to treat reproductive disorders.
We would love to hear your thoughts on this topic. Please feel free to comment below and share your experiences. If you have any questions or would like to know more about the blood-testis barrier, please ask!
What is the blood-testis barrier?
+The blood-testis barrier is a complex structure composed of multiple layers, including the basement membrane, the tight junctions between Sertoli cells, and the actin-based cytoskeleton. It serves as a physical and immunological barrier, preventing the passage of toxins, pathogens, and immune cells into the seminiferous tubules, where sperm are produced.
What is the role of sustentacular cells in the blood-testis barrier?
+Sustentacular cells, also known as Sertoli cells, play a crucial role in forming and maintaining the blood-testis barrier. They regulate the transport of essential nutrients, hormones, and growth factors to the developing sperm cells, provide structural support, and form tight junctions with neighboring cells to create a physical barrier.
What are the implications of blood-testis barrier dysfunction?
+Dysfunction of the blood-testis barrier has been implicated in various reproductive disorders, including infertility, testicular cancer, and autoimmune orchitis. Understanding the mechanisms of BTB formation and regulation is essential for developing novel therapeutic strategies to treat these disorders.