In the vast and complex landscape of healthcare, navigating the intricacies of insurance coverage can be daunting, especially when it comes to obtaining prior authorization for medical treatments. Prior authorization, also known as pre-authorization or pre-certification, is a process used by health insurance companies to determine whether they will cover a specific treatment or medication. In Texas, as in many other states, this process is crucial for ensuring that patients receive the necessary care while also controlling healthcare costs. This article delves into the specifics of the Texas prior authorization form, providing a step-by-step guide for healthcare providers, patients, and insurance companies alike.

Understanding the Purpose of Prior Authorization
Prior authorization is designed to ensure that healthcare services and medications are medically necessary and meet specific standards before they are approved for coverage. This process is beneficial for several reasons. First, it helps in preventing unnecessary medical interventions, which can reduce healthcare costs and minimize the risk of adverse reactions. Second, it allows insurance companies to negotiate prices with healthcare providers, further controlling costs. Lastly, it helps in ensuring that patients receive evidence-based care, aligning with the latest medical guidelines and research.
Benefits of Prior Authorization
- Cost Savings: By ensuring that only necessary treatments are covered, prior authorization can lead to significant cost savings for both patients and insurance companies.
- Improved Patient Safety: This process can reduce the risk of adverse reactions by ensuring that medications and treatments are appropriate for the patient's condition.
- Evidence-Based Care: Prior authorization promotes the use of treatments that are backed by scientific evidence, improving the quality of care.
How to Fill Out a Texas Prior Authorization Form
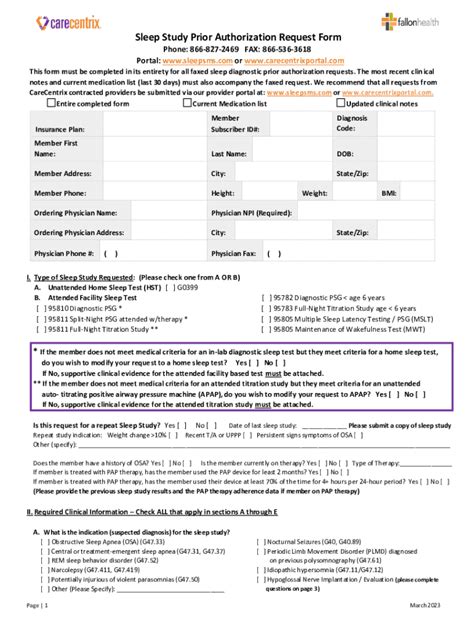
The process of filling out a Texas prior authorization form involves several steps, which are outlined below. This process typically involves the patient's healthcare provider, as they are the ones who will initiate the request for prior authorization.

Step 1: Gather Necessary Information
- Patient Details: Full name, date of birth, and insurance policy number.
- Treatment Details: Description of the treatment or medication being requested, including dosage and duration.
- Medical Necessity: A detailed explanation of why the treatment is medically necessary, often supported by medical records and test results.
Step 2: Complete the Form
- Ensure all sections of the form are completed accurately and thoroughly. Missing information can lead to delays or denials.
- The form typically includes sections for patient demographics, treatment details, and medical necessity justification.
Step 3: Submit the Form
- The completed form is usually submitted to the insurance company by the healthcare provider.
- Submission methods may vary, including online portals, fax, or mail. Check with the insurance company for their preferred method.
What Happens After Submission
After the prior authorization form is submitted, the insurance company reviews the request. This review process can vary in length but typically takes a few days to a couple of weeks. Once the review is complete, the insurance company will notify the healthcare provider of their decision.

Possible Outcomes
- Approved: The treatment or medication is covered, and the patient can proceed with the recommended care.
- Denied: The request is denied, often due to lack of medical necessity or failure to meet specific criteria. There may be an option to appeal the decision.
- Request for Additional Information: The insurance company may request more information or documentation to support the request.
Challenges and Considerations
While prior authorization is designed to ensure that patients receive necessary care while controlling costs, it can also present challenges, particularly in urgent situations where timely treatment is crucial. Healthcare providers and patients alike must navigate these complexities, ensuring that the process does not unduly delay necessary treatments.

Streamlining the Process
- Electronic Submissions: Many insurance companies now offer electronic portals for submitting prior authorization requests, which can speed up the process.
- Standardized Forms: Using standardized forms can help ensure that all necessary information is included, reducing delays.
- Open Communication: Keeping patients informed about the status of their prior authorization request can help manage expectations and reduce frustration.
Conclusion: Moving Forward with Texas Prior Authorization
Navigating the Texas prior authorization form and process requires a clear understanding of its purpose, benefits, and challenges. By following the steps outlined above and staying informed, healthcare providers, patients, and insurance companies can work together to ensure that prior authorization supports, rather than hinders, the delivery of quality healthcare in Texas.

Final Thoughts
- Collaboration is Key: Open communication and collaboration among all parties involved are crucial for a smooth prior authorization process.
- Advocacy: Patients should feel empowered to ask questions and seek support if they encounter difficulties with the prior authorization process.
- Continuous Improvement: The healthcare and insurance industries should continually seek ways to streamline and improve the prior authorization process, ensuring it serves its purpose without creating unnecessary barriers to care.
What is the purpose of prior authorization?
+Prior authorization is designed to ensure that healthcare services and medications are medically necessary and meet specific standards before they are approved for coverage.
How long does the prior authorization process typically take?
+The review process can vary in length but typically takes a few days to a couple of weeks.
What happens if a prior authorization request is denied?
+If a request is denied, there may be an option to appeal the decision. Patients should discuss this further with their healthcare provider.