Prior authorization, a crucial step in the healthcare process, can be a daunting task for patients and healthcare providers alike. The tedious process of obtaining approval from insurance companies can be overwhelming, leading to delayed treatment and frustration. However, with the introduction of SouthernScripts.Net's Prior Authorization Form, the process has become more streamlined and efficient.
Prior authorization is a necessary evil in the healthcare industry. It ensures that patients receive the necessary treatment while preventing unnecessary costs for insurance companies. However, the traditional prior authorization process is often manual, time-consuming, and prone to errors. This is where SouthernScripts.Net's innovative solution comes into play.
Streamlining the Prior Authorization Process

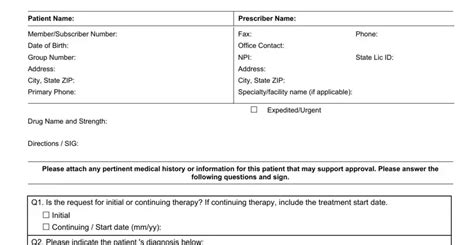
SouthernScripts.Net's Prior Authorization Form is designed to simplify the process, reducing the administrative burden on healthcare providers and patients. The online platform provides a user-friendly interface, allowing users to easily submit prior authorization requests. The form is pre-populated with patient information, reducing the risk of errors and saving time.
Benefits of Using SouthernScripts.Net's Prior Authorization Form
• Reduced Administrative Burden: The online platform automates the prior authorization process, freeing up staff to focus on patient care. • Increased Efficiency: The pre-populated form and automated submission process reduce the time spent on prior authorization requests. • Improved Accuracy: The platform minimizes the risk of errors, ensuring that requests are processed correctly the first time. • Enhanced Patient Experience: Patients receive faster approval for treatment, reducing wait times and improving health outcomes.
How SouthernScripts.Net's Prior Authorization Form Works

The prior authorization form is part of SouthernScripts.Net's comprehensive healthcare platform. Here's a step-by-step guide on how it works:
- Patient Information: The healthcare provider enters the patient's information into the platform.
- Treatment Request: The provider submits a treatment request, including the medication or procedure required.
- Prior Authorization Form: The platform generates a pre-populated prior authorization form, which is submitted to the insurance company.
- Insurance Company Review: The insurance company reviews the request and responds with an approval or denial.
- Treatment Approval: If approved, the patient can begin treatment immediately.
Case Study: Success with SouthernScripts.Net's Prior Authorization Form
A leading healthcare provider in the southern United States was struggling with the prior authorization process. They were spending an average of 30 minutes per request, resulting in delayed treatment and frustrated patients. After implementing SouthernScripts.Net's Prior Authorization Form, they saw a significant reduction in administrative time, with requests being processed in under 10 minutes. Patient satisfaction improved, and treatment outcomes increased.
The Future of Prior Authorization

As the healthcare industry continues to evolve, the prior authorization process must adapt to meet the changing needs of patients and providers. SouthernScripts.Net's innovative solution is leading the way, providing a streamlined and efficient process that benefits all parties involved.
By embracing technology and automation, the prior authorization process can be transformed from a tedious and time-consuming task to a seamless and efficient experience. As the healthcare industry moves forward, it's essential to prioritize innovation and patient-centered care.
We invite you to share your thoughts on the prior authorization process and how SouthernScripts.Net's innovative solution has impacted your healthcare experience. Please leave a comment below or share this article with your network.
What is prior authorization, and why is it necessary?
+Prior authorization is the process of obtaining approval from an insurance company before receiving medical treatment. It ensures that patients receive necessary treatment while preventing unnecessary costs for insurance companies.
How does SouthernScripts.Net's Prior Authorization Form simplify the process?
+SouthernScripts.Net's Prior Authorization Form streamlines the process by providing a user-friendly interface, pre-populated patient information, and automated submission. This reduces the administrative burden, increases efficiency, and improves accuracy.
Can I use SouthernScripts.Net's Prior Authorization Form for all types of medical treatment?
+No, SouthernScripts.Net's Prior Authorization Form is specifically designed for medication and procedure requests. However, the platform is constantly evolving to meet the changing needs of the healthcare industry.