As a healthcare provider or patient in South Carolina, you're likely familiar with the Medicaid program and its requirements. One crucial aspect of Medicaid is prior authorization, which ensures that certain medical treatments and services are medically necessary and cost-effective. In this article, we'll delve into the world of SC Medicaid prior authorization forms, providing you with a comprehensive guide to easy approval.
Understanding SC Medicaid Prior Authorization

Prior authorization is a process used by Medicaid to determine whether a specific treatment or service is necessary for a patient's condition. This process helps control healthcare costs and ensures that patients receive only the necessary care. In South Carolina, Medicaid prior authorization is required for certain services, including:
- Prescription medications
- Durable medical equipment (DME)
- Home health care
- Hospital stays
- Outpatient procedures
Benefits of SC Medicaid Prior Authorization
While prior authorization may seem like an extra step, it offers several benefits, including:
- Reduced healthcare costs: By ensuring that only necessary treatments are approved, Medicaid can control costs and allocate resources more efficiently.
- Improved patient outcomes: Prior authorization helps ensure that patients receive evidence-based treatments that are proven to be effective.
- Enhanced patient safety: By reviewing treatment plans, Medicaid can identify potential risks and prevent adverse events.
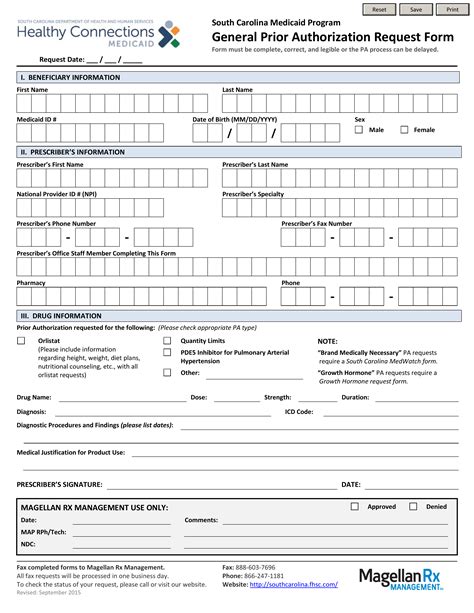
The SC Medicaid Prior Authorization Form

The SC Medicaid prior authorization form is a document that healthcare providers must complete and submit to Medicaid for review. The form typically includes the following information:
- Patient demographics
- Medical diagnosis and treatment plan
- Prescription medication information (if applicable)
- Durable medical equipment information (if applicable)
- Supporting documentation (e.g., medical records, test results)
How to Complete the SC Medicaid Prior Authorization Form
To ensure easy approval, it's essential to complete the prior authorization form accurately and thoroughly. Here are some tips to help you:
- Use the correct form: Ensure you're using the most up-to-date version of the SC Medicaid prior authorization form.
- Provide complete information: Fill out all required fields, and attach supporting documentation as needed.
- Be concise and clear: Use simple language and avoid abbreviations or acronyms.
- Submit the form promptly: Allow sufficient time for Medicaid to review and process the form.
SC Medicaid Prior Authorization Requirements

To ensure easy approval, healthcare providers must meet specific requirements when submitting prior authorization requests. These requirements include:
- Using the correct form and submitting it to the correct address
- Providing complete and accurate information
- Attaching supporting documentation as needed
- Meeting deadlines for submission and follow-up
Common SC Medicaid Prior Authorization Codes
Medicaid uses specific codes to identify prior authorization requests. Here are some common codes used in South Carolina:
- PA-01: Prescription medication prior authorization
- PA-02: Durable medical equipment prior authorization
- PA-03: Home health care prior authorization
- PA-04: Hospital stay prior authorization
- PA-05: Outpatient procedure prior authorization
SC Medicaid Prior Authorization Approval Process

Once the prior authorization form is submitted, Medicaid reviews the request to determine whether the treatment or service is medically necessary. The approval process typically involves the following steps:
- Initial review: Medicaid reviews the form for completeness and accuracy.
- Clinical review: A clinical reviewer assesses the medical necessity of the treatment or service.
- Approval or denial: Medicaid makes a determination and notifies the healthcare provider.
- Appeal process: If denied, the healthcare provider can appeal the decision.
SC Medicaid Prior Authorization Denial Reasons
If a prior authorization request is denied, it's essential to understand the reasons for denial. Common reasons for denial include:
- Lack of medical necessity
- Insufficient documentation
- Incorrect coding or billing
- Failure to meet requirements
SC Medicaid Prior Authorization Appeal Process

If a prior authorization request is denied, healthcare providers can appeal the decision. The appeal process typically involves:
- Submitting an appeal form
- Providing additional documentation or information
- A review of the appeal by a Medicaid representative
- A determination and notification of the appeal outcome
SC Medicaid Prior Authorization Tips and Best Practices
To ensure easy approval and avoid denials, follow these tips and best practices:
- Use the correct form and submit it to the correct address
- Provide complete and accurate information
- Attach supporting documentation as needed
- Meet deadlines for submission and follow-up
- Follow up with Medicaid to ensure timely processing
Conclusion: Easy SC Medicaid Prior Authorization Approval

In conclusion, SC Medicaid prior authorization is a crucial process that ensures medically necessary treatments and services are approved and covered. By understanding the requirements, completing the form accurately, and following best practices, healthcare providers can ensure easy approval and avoid denials. Remember to stay informed, follow guidelines, and appeal denials when necessary.
We encourage you to share your experiences and tips for SC Medicaid prior authorization in the comments below.
What is SC Medicaid prior authorization?
+SC Medicaid prior authorization is a process used by Medicaid to determine whether a specific treatment or service is medically necessary and cost-effective.
What is the SC Medicaid prior authorization form?
+The SC Medicaid prior authorization form is a document that healthcare providers must complete and submit to Medicaid for review.
How do I appeal a denied SC Medicaid prior authorization request?
+If a prior authorization request is denied, healthcare providers can appeal the decision by submitting an appeal form, providing additional documentation or information, and following the appeal process.