As a healthcare provider, navigating the complex world of medical billing and insurance claims can be overwhelming, especially when it comes to Anthem disputes. Anthem, one of the largest health insurance providers in the US, has its own set of rules and regulations that can often lead to disputes and denied claims. However, with the right strategies and knowledge, providers can effectively resolve Anthem disputes and ensure timely payment for their services.
Anthem disputes can arise from various issues, such as incorrect coding, insufficient documentation, or misunderstandings about coverage policies. These disputes can lead to delayed or denied payments, causing financial strain on healthcare providers. Moreover, the process of resolving these disputes can be time-consuming and labor-intensive, taking away valuable resources from patient care.
Understanding Anthem's Dispute Process

Before diving into the steps to resolve Anthem disputes, it's essential to understand the insurer's dispute process. Anthem has a multi-step process for handling disputes, which includes:
- Initial review: Anthem reviews the claim to determine if it was processed correctly.
- Reconsideration: If the claim is denied, the provider can request a reconsideration review.
- Appeal: If the reconsideration is denied, the provider can appeal the decision.
- External review: The provider can request an external review by an independent reviewer.
Step 1: Verify Patient Information and Coverage
The first step in resolving an Anthem dispute is to verify the patient's information and coverage. This includes checking the patient's demographics, policy details, and coverage dates. Ensure that the patient's information is accurate and up-to-date, as incorrect information can lead to denied claims.
Providers should also verify the patient's coverage, including the type of plan, coverage limits, and any applicable deductibles or copays. This information can be obtained through Anthem's online portal or by contacting the insurer directly.
Step 2: Review Claim Details and Coding

The next step is to review the claim details and coding to ensure accuracy. This includes checking the procedure codes, diagnosis codes, and any modifiers used. Ensure that the coding is compliant with Anthem's guidelines and industry standards.
Providers should also review the claim details, including the date of service, charge amount, and any additional information required by Anthem. This information can be obtained through Anthem's online portal or by contacting the insurer directly.
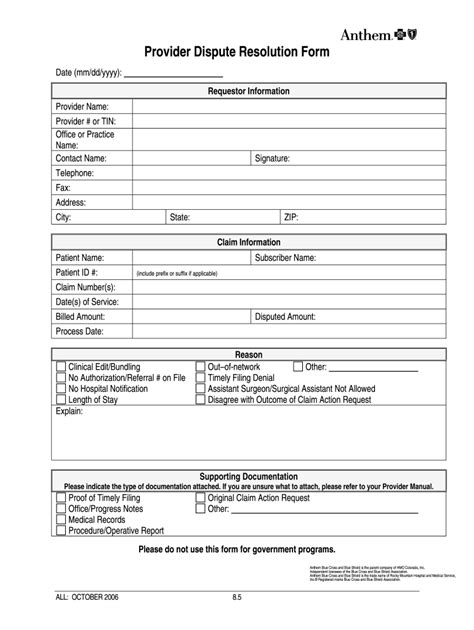
Step 3: Gather Supporting Documentation
Gathering supporting documentation is crucial in resolving Anthem disputes. This includes medical records, test results, and any other relevant information that supports the claim. Ensure that the documentation is complete, accurate, and up-to-date.
Providers should also gather any additional information required by Anthem, such as authorization forms or prior approval documentation. This information can be obtained through Anthem's online portal or by contacting the insurer directly.
Step 4: Submit a Reconsideration Request

If the claim is denied, the next step is to submit a reconsideration request. This involves providing additional information or clarification on the claim. Ensure that the request is submitted in a timely manner, as Anthem has specific deadlines for reconsideration requests.
Providers should include all relevant information and supporting documentation with the reconsideration request. This includes medical records, test results, and any other relevant information that supports the claim.
Step 5: Escalate to Appeal or External Review
If the reconsideration request is denied, the final step is to escalate the dispute to an appeal or external review. This involves providing additional information or clarification on the claim, as well as any new evidence that supports the claim.
Providers should ensure that the appeal or external review request is submitted in a timely manner, as Anthem has specific deadlines for these requests. Include all relevant information and supporting documentation with the request, and be prepared to provide additional information or clarification as needed.
Conclusion

Resolving Anthem disputes requires a strategic approach and a thorough understanding of the insurer's dispute process. By following these five easy steps, providers can effectively resolve disputes and ensure timely payment for their services.
Remember to verify patient information and coverage, review claim details and coding, gather supporting documentation, submit a reconsideration request, and escalate to appeal or external review if necessary. By taking these steps, providers can reduce the risk of denied claims and improve their overall revenue cycle management.
We invite you to share your experiences and tips on resolving Anthem disputes in the comments below. Your input can help other providers navigate the complex world of medical billing and insurance claims.
What is the first step in resolving an Anthem dispute?
+The first step is to verify patient information and coverage, including demographics, policy details, and coverage dates.
What is the purpose of submitting a reconsideration request?
+The purpose is to provide additional information or clarification on the claim, and to request that Anthem re-review the claim.
How long does it take to resolve an Anthem dispute?
+The time it takes to resolve an Anthem dispute varies, but it can take several weeks to several months, depending on the complexity of the issue and the level of escalation required.