The process of obtaining prior authorization for medical treatments and services can be a daunting task, especially when dealing with complex insurance companies like Aetna. One of the most critical steps in this process is filling out the Aetna prior authorization form, which can be overwhelming for many healthcare providers and patients. In this article, we will explore five ways to simplify the Aetna prior authorization form and make the process more efficient.
Understanding the Importance of Prior Authorization
Prior authorization is a process that requires healthcare providers to obtain approval from insurance companies before providing specific medical treatments or services. This process helps ensure that patients receive necessary care while also controlling healthcare costs. Aetna, one of the largest health insurance companies in the United States, requires prior authorization for many medical services, including surgeries, diagnostic tests, and prescriptions.

Challenges with the Aetna Prior Authorization Form
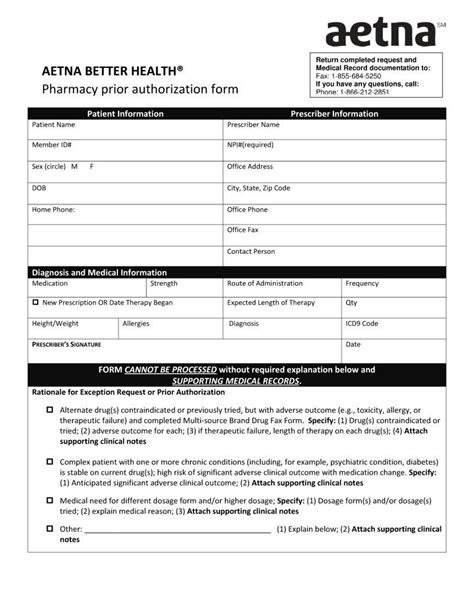
The Aetna prior authorization form can be a complex and time-consuming document to fill out, requiring detailed information about the patient's medical condition, treatment plan, and insurance coverage. Healthcare providers often struggle with the form's complexity, which can lead to delays in care and frustration for patients.
5 Ways to Simplify the Aetna Prior Authorization Form
Here are five ways to simplify the Aetna prior authorization form and make the process more efficient:
1. Use Online Prior Authorization Tools
Aetna offers online prior authorization tools that can help streamline the process. These tools allow healthcare providers to submit prior authorization requests electronically, reducing paperwork and increasing the speed of approval. Some popular online prior authorization tools include Aetna's Provider Web Portal and the Aetna Mobile App.

Benefits of Online Prior Authorization Tools
- Faster approval times
- Reduced paperwork
- Increased accuracy
- Improved communication with Aetna
2. Prepare Thoroughly Before Submitting the Form
To simplify the Aetna prior authorization form, it's essential to prepare thoroughly before submitting the form. This includes gathering all necessary documents, including the patient's medical records, test results, and treatment plans.

Tips for Preparing the Prior Authorization Form
- Gather all necessary documents
- Review the form carefully
- Ensure accurate and complete information
- Submit the form well in advance of the treatment date
3. Use Templates and Checklists
Using templates and checklists can help simplify the Aetna prior authorization form by ensuring that all necessary information is included. Aetna provides templates and checklists on its website that can be used to guide the prior authorization process.

Benefits of Using Templates and Checklists
- Increased accuracy
- Reduced errors
- Faster approval times
- Improved organization
4. Communicate Effectively with Aetna
Effective communication with Aetna is critical to simplifying the prior authorization form. This includes responding promptly to requests for additional information and following up on the status of the prior authorization request.

Tips for Communicating with Aetna
- Respond promptly to requests for additional information
- Follow up on the status of the prior authorization request
- Use clear and concise language
- Be prepared to provide additional information
5. Seek Assistance from Aetna's Provider Support Team
Aetna's provider support team is available to assist healthcare providers with the prior authorization process. This team can provide guidance on completing the prior authorization form and resolving any issues that may arise.

Benefits of Seeking Assistance from Aetna's Provider Support Team
- Expert guidance on completing the prior authorization form
- Resolution of issues and delays
- Improved communication with Aetna
- Increased efficiency
By following these five tips, healthcare providers can simplify the Aetna prior authorization form and make the process more efficient. This can lead to faster approval times, reduced paperwork, and improved patient care.
What is prior authorization, and why is it required?
+Prior authorization is a process that requires healthcare providers to obtain approval from insurance companies before providing specific medical treatments or services. It is required to ensure that patients receive necessary care while also controlling healthcare costs.
How long does the prior authorization process typically take?
+The prior authorization process typically takes several days to several weeks, depending on the complexity of the request and the responsiveness of the healthcare provider and Aetna.
What information is required on the Aetna prior authorization form?
+The Aetna prior authorization form requires detailed information about the patient's medical condition, treatment plan, and insurance coverage. This includes medical records, test results, and treatment plans.
We hope this article has provided valuable insights and tips for simplifying the Aetna prior authorization form. By following these tips, healthcare providers can make the process more efficient and improve patient care. If you have any further questions or concerns, please don't hesitate to comment below or share this article with your colleagues.