Navigating the complex world of healthcare can be overwhelming, especially when it comes to prior authorization forms. PacificSource, a leading healthcare organization, has implemented a prior authorization process to ensure that patients receive the necessary medical treatment while controlling healthcare costs. In this article, we will delve into the PacificSource prior authorization form, making it easier for you to understand and navigate the process.
The importance of prior authorization cannot be overstated. It helps prevent unnecessary medical procedures, reduces healthcare costs, and ensures that patients receive the most effective treatment for their condition. However, the process can be time-consuming and may delay medical treatment. Therefore, it is essential to understand the PacificSource prior authorization form and how to complete it efficiently.
What is PacificSource Prior Authorization Form?

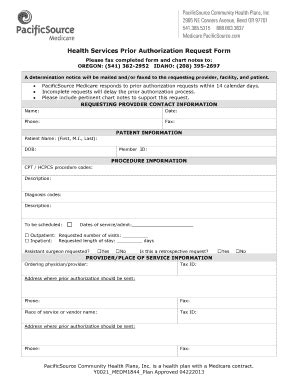
The PacificSource prior authorization form is a document that healthcare providers must complete and submit to PacificSource before performing certain medical procedures or prescribing specific medications. The form requires detailed information about the patient's condition, the proposed treatment, and the rationale behind it. PacificSource reviews the form to determine whether the treatment is medically necessary and aligns with their coverage policies.
Why is Prior Authorization Necessary?
Prior authorization is necessary for several reasons:
- It ensures that patients receive the most effective treatment for their condition.
- It helps prevent unnecessary medical procedures, reducing healthcare costs.
- It enables PacificSource to manage healthcare costs and ensure that patients receive the best possible care.
How to Complete the PacificSource Prior Authorization Form

Completing the PacificSource prior authorization form requires attention to detail and a thorough understanding of the patient's condition. Here are the steps to follow:
- Gather necessary information: Collect the patient's medical records, including diagnosis, treatment plans, and test results.
- Complete the form accurately: Fill out the form with the required information, ensuring that all fields are complete and accurate.
- Attach supporting documentation: Include any supporting documentation, such as test results or medical records, to justify the proposed treatment.
- Submit the form: Submit the completed form to PacificSource for review.
Common Mistakes to Avoid
When completing the PacificSource prior authorization form, there are several common mistakes to avoid:
- Incomplete or inaccurate information: Ensure that all fields are complete and accurate to avoid delays or denials.
- Insufficient supporting documentation: Include all necessary supporting documentation to justify the proposed treatment.
- Failure to submit the form: Submit the completed form to PacificSource in a timely manner to avoid delays in treatment.
PacificSource Prior Authorization Form Requirements

The PacificSource prior authorization form requires specific information and documentation. Here are the requirements:
- Patient information: Include the patient's name, date of birth, and contact information.
- Medical condition: Provide a detailed description of the patient's medical condition, including diagnosis and treatment plans.
- Proposed treatment: Describe the proposed treatment, including medications, procedures, or services.
- Supporting documentation: Include any supporting documentation, such as test results or medical records, to justify the proposed treatment.
What Happens After Submitting the Form?
After submitting the PacificSource prior authorization form, PacificSource will review the information to determine whether the treatment is medically necessary and aligns with their coverage policies. Here are the possible outcomes:
- Approval: PacificSource approves the treatment, and the patient can proceed with the proposed treatment.
- Denial: PacificSource denies the treatment, and the patient may need to explore alternative treatment options.
- Request for additional information: PacificSource requests additional information or documentation to support the proposed treatment.
PacificSource Prior Authorization Form FAQs

Here are some frequently asked questions about the PacificSource prior authorization form:
- What is the purpose of the PacificSource prior authorization form?: The form is used to determine whether a proposed treatment is medically necessary and aligns with PacificSource's coverage policies.
- How long does the prior authorization process take?: The prior authorization process typically takes 2-5 business days, but may take longer in some cases.
- Can I appeal a denied prior authorization?: Yes, you can appeal a denied prior authorization by submitting additional information or documentation to support the proposed treatment.
Conclusion
In conclusion, the PacificSource prior authorization form is an essential document that healthcare providers must complete and submit to PacificSource before performing certain medical procedures or prescribing specific medications. By understanding the form requirements and avoiding common mistakes, healthcare providers can ensure that patients receive the necessary medical treatment while controlling healthcare costs. If you have any questions or concerns about the PacificSource prior authorization form, please don't hesitate to reach out to PacificSource or your healthcare provider.
What is the purpose of the PacificSource prior authorization form?
+The form is used to determine whether a proposed treatment is medically necessary and aligns with PacificSource's coverage policies.
How long does the prior authorization process take?
+The prior authorization process typically takes 2-5 business days, but may take longer in some cases.