OptumRx is a leading pharmacy benefit management organization that provides prescription medication management services to millions of people across the United States. One of the essential processes in managing prescription medications is prior authorization, which ensures that patients receive the most effective and cost-efficient treatments. In this article, we will delve into the world of OptumRx prior authorization and provide a step-by-step guide on how to navigate the process using the OptumRx prior authorization request form.
Understanding OptumRx Prior Authorization
Prior authorization is a process used by pharmacy benefit managers like OptumRx to ensure that prescription medications are medically necessary and cost-effective. The process involves reviewing a patient's medical history, diagnosis, and treatment plan to determine whether a specific medication is necessary. This process helps to prevent unnecessary costs, reduces waste, and ensures that patients receive the most effective treatments.

Why is Prior Authorization Necessary?
Prior authorization is essential for several reasons:
- Ensures medically necessary treatments: Prior authorization ensures that patients receive treatments that are medically necessary and aligned with their diagnosis and treatment plan.
- Reduces unnecessary costs: By reviewing treatment plans and medications, prior authorization helps to prevent unnecessary costs and reduce waste.
- Prevents adverse interactions: Prior authorization helps to identify potential adverse interactions between medications and ensures that patients are not taking contraindicated medications.
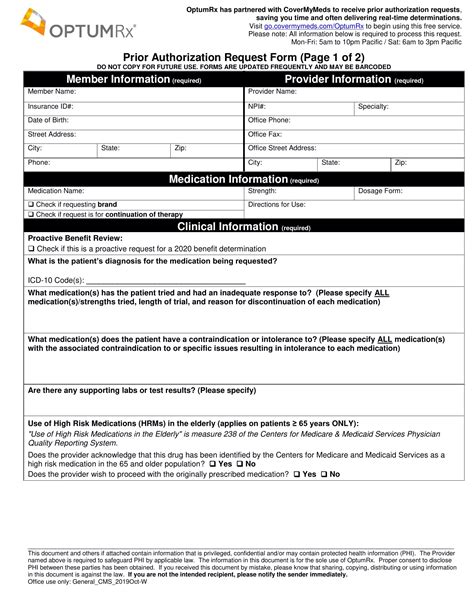
The OptumRx Prior Authorization Request Form
The OptumRx prior authorization request form is a crucial document that healthcare providers use to request prior authorization for their patients. The form requires providers to submit detailed information about the patient's medical history, diagnosis, treatment plan, and medications.

Step-by-Step Guide to Completing the OptumRx Prior Authorization Request Form
Completing the OptumRx prior authorization request form requires careful attention to detail and accurate information. Here is a step-by-step guide to help healthcare providers navigate the process:
- Section 1: Patient Information
- Provide the patient's name, date of birth, and member ID number.
- Ensure that the patient's information is accurate and matches their identification documents.
- Section 2: Prescriber Information
- Provide the prescriber's name, DEA number, and contact information.
- Ensure that the prescriber's information is accurate and up-to-date.
- Section 3: Medication Information
- List the medication(s) being requested, including the dosage, frequency, and duration of treatment.
- Provide the NDC number and the medication's generic name.
- Section 4: Medical History and Diagnosis
- Provide a detailed medical history, including the patient's diagnosis, symptoms, and test results.
- Ensure that the medical history is accurate and up-to-date.
- Section 5: Treatment Plan and Rationale
- Describe the treatment plan and rationale for the requested medication.
- Provide evidence-based guidelines and clinical trials that support the treatment plan.
Submitting the OptumRx Prior Authorization Request Form
Once the OptumRx prior authorization request form is complete, healthcare providers can submit it to OptumRx for review. Providers can submit the form via:
- Fax: 1-800-711-4555
- Phone: 1-800-711-4555
- Online: OptumRx website

What to Expect After Submitting the Form
After submitting the OptumRx prior authorization request form, healthcare providers can expect the following:
- Review Process: OptumRx will review the request form and may contact the provider for additional information.
- Determination: OptumRx will make a determination regarding the prior authorization request and notify the provider via phone or fax.
- Approval or Denial: If approved, the patient's medication will be covered. If denied, the provider can appeal the decision.
Avoiding Common Mistakes
To ensure a smooth prior authorization process, healthcare providers should avoid common mistakes, such as:
- Incomplete or inaccurate information
- Missing or incomplete documentation
- Failure to provide evidence-based guidelines and clinical trials

Best Practices for a Successful Prior Authorization Process
To ensure a successful prior authorization process, healthcare providers should:
- Ensure accurate and complete information
- Provide detailed medical history and diagnosis
- Include evidence-based guidelines and clinical trials
- Submit the form via the most efficient method (online or phone)
By following these best practices and using the step-by-step guide provided in this article, healthcare providers can navigate the OptumRx prior authorization process with ease and ensure that their patients receive the most effective and cost-efficient treatments.
What is prior authorization?
+Prior authorization is a process used by pharmacy benefit managers like OptumRx to ensure that prescription medications are medically necessary and cost-effective.
How do I submit the OptumRx prior authorization request form?
+Providers can submit the form via fax, phone, or online through the OptumRx website.
What happens after I submit the form?
+OptumRx will review the request form and may contact the provider for additional information. They will then make a determination regarding the prior authorization request and notify the provider via phone or fax.
We hope this article has provided you with a comprehensive understanding of the OptumRx prior authorization process and the steps required to complete the prior authorization request form. If you have any further questions or concerns, please don't hesitate to reach out to us.